At a glance
Fraudulent claims create financial losses and erode customer trust for insurers.
A strong fraud detection workflow identifies suspicious signals, triages cases quickly, and routes genuine ones to SIU for investigation.
Effective workflows balance fraud prevention with seamless experiences for honest policyholders.
Moxo automates case routing, evidence capture, and multi-party investigations within a secure, audit-ready portal.
The evolving landscape of insurance fraud detection
Insurance fraud costs U.S. consumers an estimated $308.6 billion every year. From exaggerated claims to entirely fabricated incidents, fraudulent activities not only impact insurers' bottom lines but also drive up premiums for everyone. As fraudsters become more sophisticated, traditional detection methods are struggling to keep pace. This makes it crucial for claims handlers and Special Investigation Units (SIUs) to adopt smarter, more efficient strategies.
This guide explores a modern approach to claims fraud detection. We'll cover how to identify critical fraud signals, effectively triage suspicious cases for investigation, and leverage automation to streamline and enhance your SIU workflows, helping you stay one step ahead of emerging threats.
Why fraud detection workflows matter
Insurance fraud is a significant and growing challenge, costing the U.S. more than $308 billion annually (Coalition Against Insurance Fraud). Beyond the staggering financial impact, unchecked fraud damages policyholder trust, undermines regulatory compliance, and increases premiums for honest customers. Without effective fraud detection workflows, insurers risk reputational harm, customer dissatisfaction, and potential legal penalties.
Traditional claims review processes often rely on outdated methods like manual checks, rigid rules, or siloed tools that don’t communicate with each other. These inefficiencies slow down claim approvals, frustrate customers, and create blind spots where fraud can slip through. Moreover, with the increasing sophistication of fraud schemes, traditional methods are no longer sufficient to detect subtle or emerging patterns.
A well-structured claims fraud detection workflow is essential. It ensures that potential fraud signals are captured at the point of intake, triaged consistently with clear criteria, and referred for deeper investigation when necessary. By leveraging modern tools such as AI, data analytics, and automated workflows, insurers can streamline this process, improving both accuracy and speed.
Key components of an effective fraud detection workflow
- Signal detection at intake: Use advanced AI to flag anomalies, such as repeated claims, inconsistent information, or unusual patterns, right at the start.
- Integrated triage process: Implement a consistent and automated approach to sort high-risk cases from legitimate ones, reducing false positives while ensuring thorough reviews.
- Automation in special investigative unit (SIU) workflows: Automate repetitive tasks in fraud investigations, like gathering data, cross-checking records, or generating reports, freeing up SIU teams to focus on complex cases.
- Continuous learning: Leverage machine learning models that adapt to new fraud patterns over time, improving detection accuracy and keeping up with evolving schemes.
By adopting these workflows, insurers can protect themselves against financial losses, maintain policyholder trust, and deliver a seamless claims experience for genuine customers. A proactive approach to fraud detection not only safeguards the bottom line but also strengthens the insurer’s position as a trusted and reliable partner.
Identifying fraud signals and setting triage rules
Fraud signals are the "red flags" that indicate a claim deserves closer scrutiny. These aren't always definitive proof of fraud but rather indicators that suggest deeper investigation is warranted. They might include inconsistencies, unusual patterns, or behaviors that deviate from historical norms.
Key examples of fraud signals
Inconsistent claimant data: Mismatched addresses, conflicting personal details, or frequent policy changes occurring just before a claim is filed.
Suspicious timing: Claims submitted unusually soon after a policy is purchased, or incidents reported right before policy expiration.
Duplicate or inflated billing: Multiple providers submitting identical or exaggerated charges for the same treatment or service.
Network anomalies: A high volume of claims linked to a specific adjuster, doctor, repair shop, or attorney, potentially indicating organized fraud.
Behavioral cues: A claimant's reluctance to provide details, an overly aggressive demeanor, or inconsistencies in their story.
Geographic hotspots: Claims originating from areas with a known history of fraudulent activity.
Past fraud history: Any previous involvement of the claimant or associated parties in fraudulent claims.
Once these signals are detected, triage rules determine the appropriate next steps. Not every flagged claim requires the same level of intervention. Triage ensures that resources are allocated efficiently, escalating high-risk cases while fast-tracking low-risk ones.
Effective triage involves
Scoring and weighting: Assigning scores to different signals based on their potential impact, creating a cumulative risk score for each claim.
Defining thresholds: Establishing clear thresholds for what constitutes a low, medium, or high-risk claim, guiding automated actions.
Automated routing: Using workflow automation to immediately route claims that meet certain high-risk criteria to the Special Investigations Unit (SIU) for in-depth analysis.
Setting SLAs: Defining service level agreements for how quickly different risk-level claims should be processed or investigated.
Requesting additional documentation: For medium-risk claims, the system might automatically request further evidence or details before moving forward.
By leveraging workflow automation, insurers can define these thresholds, set robust SLAs, and ensure that no high-risk claim slips through the cracks, optimizing both efficiency and fraud detection accuracy.
SIU referral & case building: Automating the deep dive
Once initial fraud detection signals have been analyzed and high-risk claims triaged, the next critical step is referring them to the Special Investigation Unit (SIU). This isn't just a simple handoff; it's the structured process of building a robust case, ensuring every piece of evidence supports a potential fraud claim. Automating aspects of this SIU workflow is crucial for efficiency and accuracy.
A streamlined SIU process typically includes:
Expert assignment: Automatically routing claims to investigators with the specific expertise required for the type of fraud suspected.
Automated document collection: Leveraging technology to efficiently gather and organize supporting documents, such as medical reports, repair invoices, police records, and digital communications, reducing manual effort and potential oversight.
Interview management: Streamlining the scheduling and recording of interviews with claimants, witnesses, or providers, with automated transcription and storage for easy access.
Digital case file creation: Building a comprehensive, centralized digital case file that automatically tracks every action, document, and communication, ensuring compliance and an unimpeachable audit trail.
Without a structured, and ideally automated, workflow, these essential steps can become fragmented across emails, spreadsheets, and phone calls. This disorganization inevitably leads to missed evidence, duplicated efforts, and costly leakage, undermining the entire fraud detection effort.
Interviews & evidence collection
Evidence collection is where workflows often break down. Missing documents or unverifiable statements can derail an investigation. A well-designed workflow supports investigators with:
- Secure document requests that ensure sensitive files (e.g., medical records) are uploaded into a compliant system.
- E-signatures and digital forms to capture consent or witness statements.
- Audit trails to prove when and how evidence was collected.
Consider a real-world example: An insurer investigating staged auto accidents required police reports and witness affidavits. By centralizing these in a secure document collection workflow, investigators cut case resolution time by weeks while reducing email exposure.
Interviews & evidence collection in fraud detection
Evidence collection is a critical stage in fraud detection workflows, often where inefficiencies arise. Missing documents, unverifiable statements, or disorganized evidence can delay investigations or even compromise their success. To combat this, a well-designed workflow can significantly enhance the efficiency and reliability of evidence collection, ensuring fraud cases are handled swiftly and accurately.
Key elements of an optimized evidence collection process
Secure document requests: sensitive files such as medical records, invoices, or repair estimates should be uploaded to a compliant system where they are protected and easily accessible.
E-signatures and digital forms: simplify the process of capturing consent, sworn affidavits, or witness statements while maintaining legal compliance.
Audit trails: maintain irrefutable records of when, how, and by whom evidence was collected to ensure the integrity of the investigation.
For example, consider an insurer investigating staged auto accidents. These cases often require police reports, repair invoices, and witness affidavits to build a case. By implementing a secure and centralized document collection workflow, investigators not only reduced email exposure but also cut case resolution times by weeks.
Enhancing interviews as part of fraud detection
Interviews with claimants, witnesses, or involved parties also play an integral role in fraud detection. Structured and well-documented interviews can help identify inconsistencies, uncover false claims, and strengthen the case.
Tips to streamline and enhance the interview process
- Use interview templates to ensure all relevant questions are covered and align with fraud indicators.
- Record interviews (with consent) for later review and transcription.
- Leverage speech analytics tools to detect hesitation, inconsistencies, or stress signals that may indicate deception.
- Combine interview findings with other collected evidence, like document discrepancies or metadata analysis, to piece together a complete picture of the fraud attempt.
By automating parts of the evidence collection and interview process through specialized SIU (Special Investigations Unit) workflows, insurers can allocate resources more efficiently, focus on high-priority cases, and reduce the risk of fraudulent claims slipping through the cracks.
Decisions and outcomes: The final verdict
Every fraud investigation concludes with one of three primary outcomes: confirming fraud, clearing the claim for payment, or marking the case as inconclusive. An automated workflow is essential to ensure these outcomes are handled efficiently and ethically.
A well-structured system ensures these outcomes are:
- Transparent: All investigation steps are logged and timestamped, creating a clear audit trail for reviews and compliance.
- Consistent: Standardized automation ensures similar signals and evidence lead to consistent, unbiased decisions for all policyholders.
- Actionable: The system triggers immediate actions: flagging fraudulent claims, fast-tracking valid ones, and tracking inconclusive cases.
Measuring success and proving value
To optimize the fraud detection process, insurers must track key performance indicators (KPIs). Critical metrics include:
Cycle time: How long does it take to resolve a case from the initial flag to the final outcome?
Severity of fraud: What is the monetary value of the fraud detected and prevented?
Leakage percentage: How much money is paid out on fraudulent or inflated claims that were not caught?
Re-open rates: How often are claims re-opened after an initial decision?
Tracking these metrics does more than just measure fraud risk. It allows insurers to quantify the ROI of their fraud detection technology and prove operational efficiency to regulators and reinsurers, ultimately building a more resilient and trustworthy claims process.
Build it in Moxo: Step-by-step
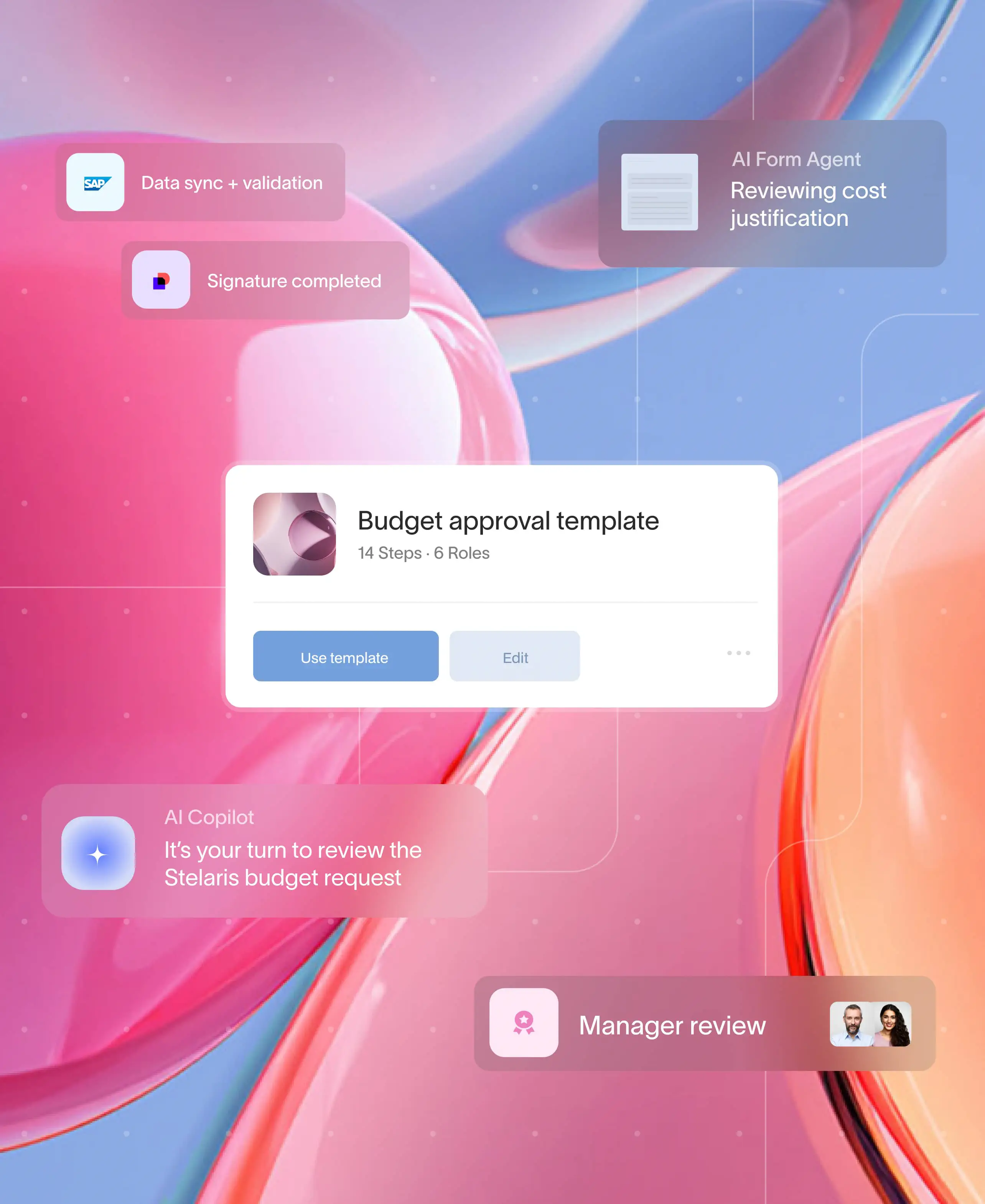
Moxo transforms this process into a secure, automated, client-facing workflow that reduces friction while ensuring compliance.
Flow builder
Design workflows with no-code tools: request files, capture form data, route to underwriters, or collect eSignatures.
Controls
Set up decision branches, SLAs, and thresholds. For example, auto-approve claims under $1,000 if confidence is above 90%.
Automations and integrations
Connect to policy admin systems, CRMs, payments, or e-sign providers like DocuSign and Jumio.
Magic links for external participants
Invite policyholders, brokers, vendors, or providers to securely upload documents and track status through a client portal without needing a login.
AI agents (coming soon)
Agents can prefill forms, answer policyholder questions, or review evidence packets for accuracy.
Management reporting
Track metrics like straight-through processing %, claim severity, cycle time, or re-open rates. Segment by line of business dashboards or region.
Governance
Moxo ensures SOC 2, GDPR, and HIPAA compliance with encryption, SSO, and full evidence exports.
Moxo makes it easier
Insurers worldwide trust Moxo to orchestrate high-stakes workflows like fraud detection. Unlike internal-only project tools, Moxo provides a branded, secure client portal where external parties (policyholders, brokers, providers) can collaborate without exposing sensitive data to email.
With Moxo, insurers see:
- 40–60% faster approvals with automated routing.
- 75% more case capacity for SIU investigators
- 95% less email exposure, improving compliance posture.
Case in point: A leading claims consulting firm adopted Moxo’s document collection and client portal, reducing claim cycle times while satisfying strict regulatory audit requirements.
Strengthen your workflows
Fraud detection workflows are the insurer’s immune system. By combining signals, triage, SIU investigation, and evidence management, insurers can control risk without sacrificing speed.
Moxo strengthens these workflows with automation, compliance, and branded portals, enabling insurers to protect both their bottom line and their policyholders’ trust. The result is faster decisions, stronger ROI, and a framework ready for regulators.
Ready to explore? Book a demo with Moxo and see how secure, automated workflows can modernize your fraud detection approach.
FAQs
What is a claims fraud detection workflow?
It’s a structured process that helps insurers identify suspicious claims, triage them, and escalate for investigation while ensuring compliance.
Why is SIU referral important in fraud detection?
SIU referral ensures suspicious claims are investigated by specialists, with evidence and interviews captured in a defensible way.
Can technology improve fraud detection?
Yes. Platforms like Moxo automate routing, capture documents securely, and maintain audit trails regulators require.
Is fraud detection just about technology?
No. It combines human expertise with technology — investigators interpret evidence, while workflows ensure consistency and compliance.
How does Moxo differ from internal project tools?
Would you invite a client or policyholder into Asana or Trello? With Moxo, you can — because it’s a secure, branded portal designed for external collaboration.