.png)
At a glance
The claims processing workflow determines how efficiently insurers handle and resolve customer requests.
Well-structured workflows reduce cycle times, improve accuracy, and strengthen policyholder trust.
Roles, decisions, and SLAs guide each step—from adjudication and reserve setting to payments and recoveries.
Moxo helps insurers transform static process maps into live, automated workflows for faster, compliant claim resolution.
Demystifying the claims workflow
Claims processing often evokes images of tedious paperwork, manual approvals, and long wait times. But in today’s digital era, customers expect instant updates and frictionless experiences — even in complex processes like insurance claims.
For insurers, every claim is a test of credibility. A single delay can erode years of brand trust, while inefficiencies quietly bleed profits through rework, leakage, and compliance risks. The question isn’t just how fast a claim can be paid — it’s how intelligently it can be processed from intake to payout.
This article breaks down the modern claims processing workflow step by step — showing how automation, clear roles, and workflow orchestration can turn a high-friction process into a strategic advantage.
Why claims workflows matter now
Insurance is built on trust, and that trust is most tested when a customer files a claim. This is the moment of truth for insurers: the point at which policyholders expect their insurer to deliver on its promises. However, delays in claims processing remain one of the biggest drivers of customer dissatisfaction. According to McKinsey, 60% of insurers cite inefficiencies in claims workflows as their top challenge.
A fragmented workflow creates ripple effects:
- Delays in adjudication and payment cycles
- Missed SLA targets and regulatory risks
- Inconsistent documentation and data silos
- Escalating claims leakage
On the flip side, an automated, well-structured workflow ensures speed, accuracy, and compliance — creating a transparent experience for both adjusters and policyholders.
With modern workflow tools like Moxo, insurers can embed intelligence and accountability into each stage — automating escalations, enforcing SLAs, and integrating policy systems for end-to-end visibility.
The complete claims processing workflow
1. First notice of loss (FNOL): intake and verification
The workflow begins the moment a claim is reported. The insurer collects basic details like policy number, incident date, and supporting evidence.
A digital FNOL system ensures:
- Seamless intake through forms or mobile uploads
- Instant acknowledgment to the policyholder
- Auto-validation of policy data
A strong FNOL foundation sets the tone for the rest of the claim, minimizing manual entry and eliminating back-and-forth follow-ups.
2. Claims triage: routing and prioritization
After intake, each claim is categorized based on complexity, value, and potential fraud risk.
Automated triage enables:
- Straight-through processing for simple claims
- Routing complex cases to specialized adjusters
- Auto-flagging anomalies using AI or pattern detection
With automation, insurers can reduce triage time from days to minutes, ensuring the right cases reach the right hands instantly.
3. Investigation and documentation
Once categorized, claims enter the verification phase. Here, adjusters collect documents, assess damages, and engage third parties if needed.
Digital workflows help by:
- Automating document requests with deadlines
- Logging every communication and approval
- Tracking evidence for audits
By digitizing this step, insurers prevent data loss and keep investigations transparent — critical for both compliance and customer satisfaction.
4. Adjudication: ensuring fairness and compliance
Adjudication determines whether the claim is payable under the policy. This step balances automation and human judgment.
- Automation: Flags limits, checks prior claims, detects policy overlaps.
- Human oversight: Validates context and fairness.
For instance, firms using Moxo’s adjudication workflows report up to 40% faster reviews while reducing manual rework and maintaining audit readiness.
5. Reserve setting and financial tracking
Setting reserves is vital for financial accuracy and solvency compliance. However, reserves often evolve as new information emerges.
An effective workflow should include:
- Initial reserve setup at intake based on claim severity
- Auto-reminders to update reserves when new data arrives
- Audit trails and approval logs
Embedding these controls within an automated platform ensures consistency and transparency for both finance and regulatory reporting.
6. Payment processing and closeout
The payment phase is the “moment of truth” — where customer satisfaction peaks or plummets.
Common friction points include manual approvals, payment delays, or lack of visibility.
A modern claims workflow integrates with payment systems, allowing insurers to:
- Process disbursements automatically after approval
- Sync financial data across departments
- Notify customers instantly via client portals
With Moxo, insurers can offer a branded, mobile-first portal where clients track payment status and download receipts, reducing inbound calls by up to 75%.
7. Recoveries and subrogation
Not all claims end at payout. Many require recoveries or subrogation against third parties.
Automating this stage prevents lost opportunities and missed deadlines.
- Auto-trigger recovery tasks post-payment
- Route documentation to legal or collections
- Use dashboards to monitor recovery rates
This ensures that financial recoveries are systematic, not situational, helping insurers improve profitability without increasing headcount.
8. Post-claim analytics and optimization
After every claim is closed, data analysis reveals process trends and cost drivers.
With integrated reporting, insurers can:
- Track SLA compliance and adjust staffing
- Identify recurring claim types or fraud risks
- Benchmark performance across business lines
Continuous improvement transforms claims management from reactive firefighting to proactive strategy.
Map roles, steps, decisions & SLAs
Every claim involves multiple actors — policyholders, adjusters, supervisors, and often third-party vendors. Mapping these roles early ensures responsibilities are clear. For example, defining who verifies documentation versus who approves reserves can reduce handoff delays.
Equally important are SLAs. When insurers set clear expectations — for example, “acknowledge FNOL within 24 hours” — it creates accountability. These agreements should be embedded directly into the workflow, so if a step exceeds SLA, escalation is automatic.
A simple analogy: think of claims like an airport runway. Planes can land safely only when each role — tower, crew, ground staff — is synchronized by clear rules and timing. Without it, gridlock and safety risks occur.
Adjudication checks & approvals
Adjudication ensures that a claim is valid, within coverage, and free of fraud. This step often requires both automation and human judgment.
- Automated systems can flag policy limits, cross-check prior claims, or detect anomalies.
- Adjusters add context, such as reviewing evidence from police reports or medical documentation.
Firms that embed adjudication into the workflow see reduced errors and faster decision-making. For example, Shields Tax CPA used Moxo’s workflow automation to cut review times by 40%, ensuring compliance without bottlenecks.
Reserve setting & updates
Setting reserves is both an art and a science. Regulators require reserves to be established early, yet claims evolve over time. The workflow should allow for:
- Initial reserve allocation based on case severity.
- Updates when new information arrives (e.g., additional medical bills).
- Audit trails to ensure transparency for regulators.
Without clear controls, reserve updates can be inconsistent, impacting financial reporting. Embedding approval workflows with audit logs ensures each change is visible and regulator-ready.
Payment & closeout
The moment of truth in any claim is the payout. Payments should be seamless, but legacy systems often introduce friction. Common challenges include:
- Duplicate checks caused by manual entry.
- Delays in approval chains.
- Lack of transparency for policyholders.
Modern workflows integrate with payment rails to release funds directly, while also updating all stakeholders. A branded client-facing portal ensures customers can track status, view payment receipts, and receive closure notifications — reducing inbound calls by up to 75%.
Recoveries & subrogation handoff
Claims don’t always end with payment. Recoveries, such as subrogation against a third party, require structured handoffs. If these are manual, insurers risk losing recovery opportunities.
Embedding branching workflows ensures recovery tasks are triggered automatically, with documentation routed to legal or collections teams. Reporting dashboards then track recovery rates, helping insurers reduce leakage.
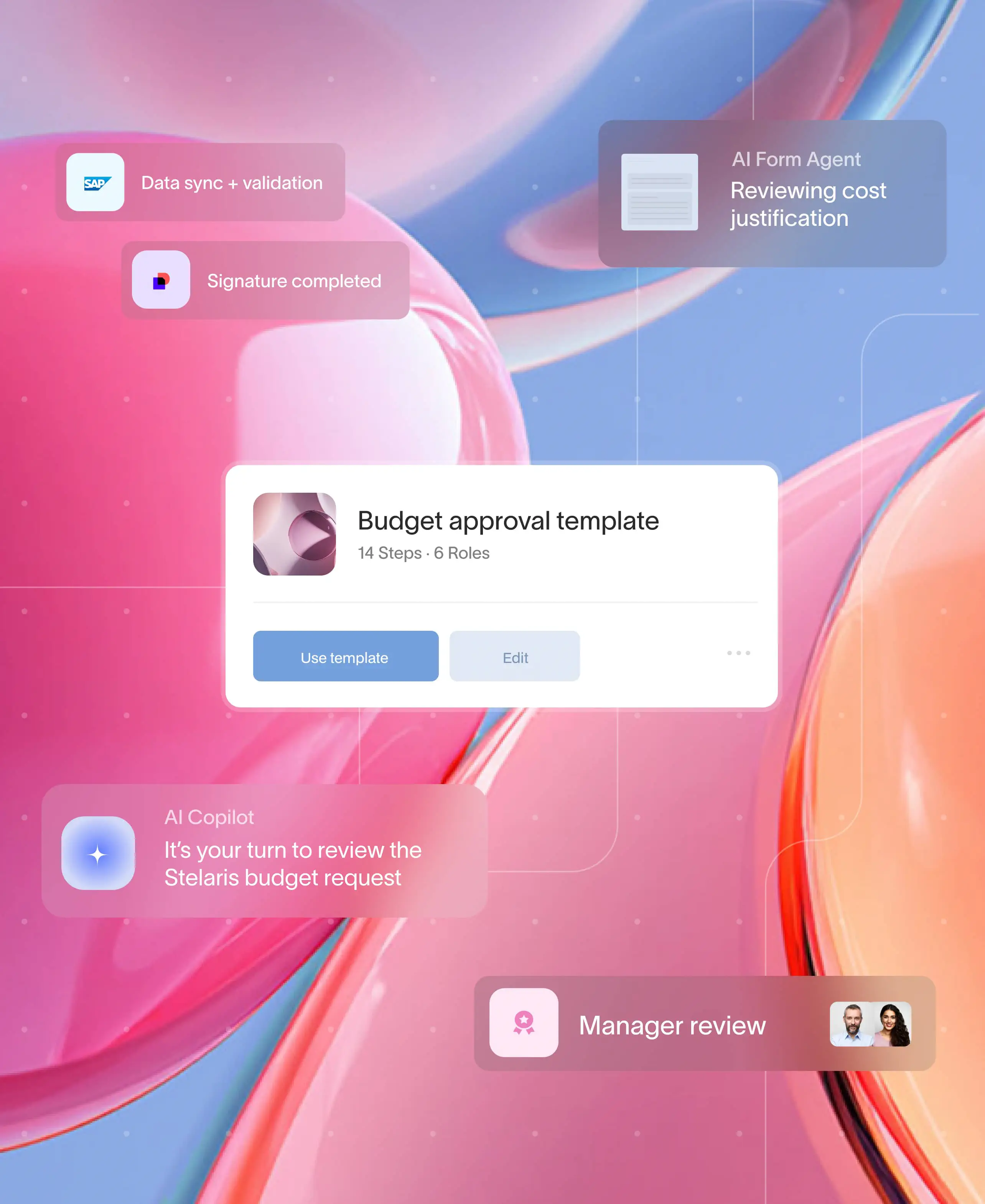
Build it in Moxo (step by step)
Flow Builder
Moxo provides a no-code workflow builder for intake forms, file requests, approvals, and e-signatures. Claims leaders can map FNOL to closeout without writing a single line of code.
Controls
Branching logic, decision milestones, and SLA thresholds allow teams to build escalation into the workflow. For example, if medical documentation isn’t received within three days, Moxo can auto-notify the adjuster — all managed within customized workflows.
Automations & Integrations
Moxo integrates with policy admin and claims core systems, CRMs, DocuSign, Jumio, and payment providers to avoid double data entry and reduce errors.
Magic Links for External Participants
Policyholders, brokers, or vendors can join the process securely through magic links, without needing a full login. This keeps the workflow both secure and accessible.
Management Reporting
Performance dashboards track cycle times, straight-through processing rates, claim severity, leakage, and recovery performance. Leaders can filter by line of business, region, or channel to spot patterns.
Governance
Moxo ensures SOC 2, GDPR, HIPAA, and PHI compliance with SSO/SAML, role-based access, encryption, and audit trails. Evidence can be exported for regulators with one click.
How Moxo helps
Moxo enables insurers to move from static process maps to live, automated workflows that orchestrate every claim from intake to payment. Its workflow automation capabilities, client portals, and secure compliance features help firms deliver:
- 40–60% faster approvals with automated SLAs and escalations.
- 75% greater client capacity by reducing manual follow-ups.
- 95% fewer emails, as all interactions live inside the portal.
- A branded, mobile-first experience that builds trust.
Case in point: Zeta Global leveraged Moxo to streamline client-facing workflows, cutting approval times significantly while maintaining compliance.
Bringing it all together
The claims processing workflow is more than a back-office function, it’s the backbone of customer trust and operational efficiency. By digitizing every touchpoint from FNOL to recovery, insurers gain agility, accuracy, and control.
Moxo acts as the orchestration layer connecting systems, people, and customers. It brings together workflow automation, collaboration, and compliance into one secure environment. Insurers can design, execute, and monitor end-to-end claims processes without coding — ensuring speed, accuracy, and transparency.
Modernize your claims process with Moxo. See how top insurers use Moxo to cut processing times, improve compliance, and elevate client experience. Book a personalized demo today.
FAQs
What is a claims processing workflow?
It’s the step-by-step process insurers use to handle claims — from intake to adjudication, payment, and closeout.
How do SLAs improve claims processing?
SLAs set time-bound expectations. With Moxo, SLAs can trigger automated escalations, ensuring no claim falls through.
Can clients track their claims online?
Yes. With a client portal, customers can submit documents, track status, and receive updates in real time.
What compliance requirements apply to claims workflows?
Insurers must comply with regulations like SOC 2, GDPR, HIPAA. Moxo’s audit trails and encryption make compliance easier.
Does Moxo replace my claims system?
No. Moxo complements policy admin and claims systems, serving as the orchestration layer for external participants and workflow automation.