.webp)
At a glance
Claims automation software closes the gaps left by traditional systems in external workflows, fraud detection, and reporting.
It streamlines document validation, fraud triage, approvals, and reporting across human and automated steps.
The right platform accelerates approvals, increases adjuster capacity, and reduces email communication.
Moxo enables insurers to manage claims securely and efficiently with automated, client-facing workflows built for speed and compliance.
Why claims automation matters
In today's competitive landscape, efficiency is key. Handling claims manually is not only time-consuming but also prone to errors, leading to increased costs and unhappy customers. Claims automation software can transform this process, using technology to handle claims faster, more accurately, and at a lower cost. This allows your team to focus on more complex cases and improve customer satisfaction. However, with so many options available, choosing the right software can be overwhelming. This guide will walk you through the key factors to consider, helping you select the best claims automation solution for your business needs.
The urgency of modern claims
The urgency of modern claims is undeniable. The insurance industry loses billions annually to inefficiencies. McKinsey highlights that claims automation can slash operational costs by 30% while simultaneously boosting accuracy and customer satisfaction. Despite these clear benefits, many carriers still grapple with outdated methods like email chains, spreadsheets, and legacy systems to coordinate between policyholders, brokers, vendors, and adjusters. This leads to delays, increased costs, and frustrated customers.
While core claims systems like Guidewire or Duck Creek are foundational, they were never built to handle the complexities of external collaboration, real-time document validations, or sophisticated fraud detection and triage. This crucial gap is precisely why forward-thinking insurers are now investing in specialized claims automation software. This new category of solutions is designed to complement, not replace, existing core systems by orchestrating secure, auditable, and efficient workflows. Choosing the right claims automation software isn't just about reducing costs; it's about transforming the entire claims experience, improving customer loyalty, and gaining a competitive edge.
The problem with claims processing today
Despite significant investments in digitization, the insurance claims process remains riddled with inefficiencies. Many insurers find themselves in a state of "digital deadlock," where new technologies have been layered onto outdated workflows, failing to deliver the expected returns. This results in persistent challenges that slow down operations, increase costs, and expose businesses to risk.
The insurance industry faces three key problems:
- Manual processes: Adjusters waste time on administrative tasks, creating bottlenecks and diverting from essential work like claim evaluation.
- Fragmented tools: Insurers use many disconnected tools, leading to data silos, manual transfers, errors, and no single view of a claim.
- Compliance risks: Manual, fragmented systems make it hard to maintain audit trails, increasing exposure to regulatory penalties and reputational damage.
These inefficiencies are a direct cause of **claims leakage**—the money an insurer loses through avoidable overpayments, fraud, and administrative mismanagement. A 2023 Accenture study highlights the scale of this issue, noting that leakage can account for 6–10% of total claims costs. For an insurer with $1 billion in annual claims, that translates to a staggering potential loss of up to $100 million. This isn't just a line item on a balance sheet; it's a critical drain on profitability that impacts the entire business.
What category are you buying
Understanding the different types of insurance technology is crucial for choosing the right claims automation solution for your business. Not all insurance technology fits the same need, and selecting incorrectly can lead to inefficiencies or incomplete solutions:
Key features to look for
When evaluating claims automation software, look beyond buzzwords and focus on the capabilities that truly impact operational performance. The right platform should unify processes, streamline communication, and ensure complete auditability across every stage of the claims lifecycle.
1. End-to-end workflow automation
The best platforms automate the full claims journey — from First Notice of Loss (FNOL) to adjudication, payout, and subrogation. This ensures every participant, task, and document moves through one connected system instead of scattered spreadsheets or emails.
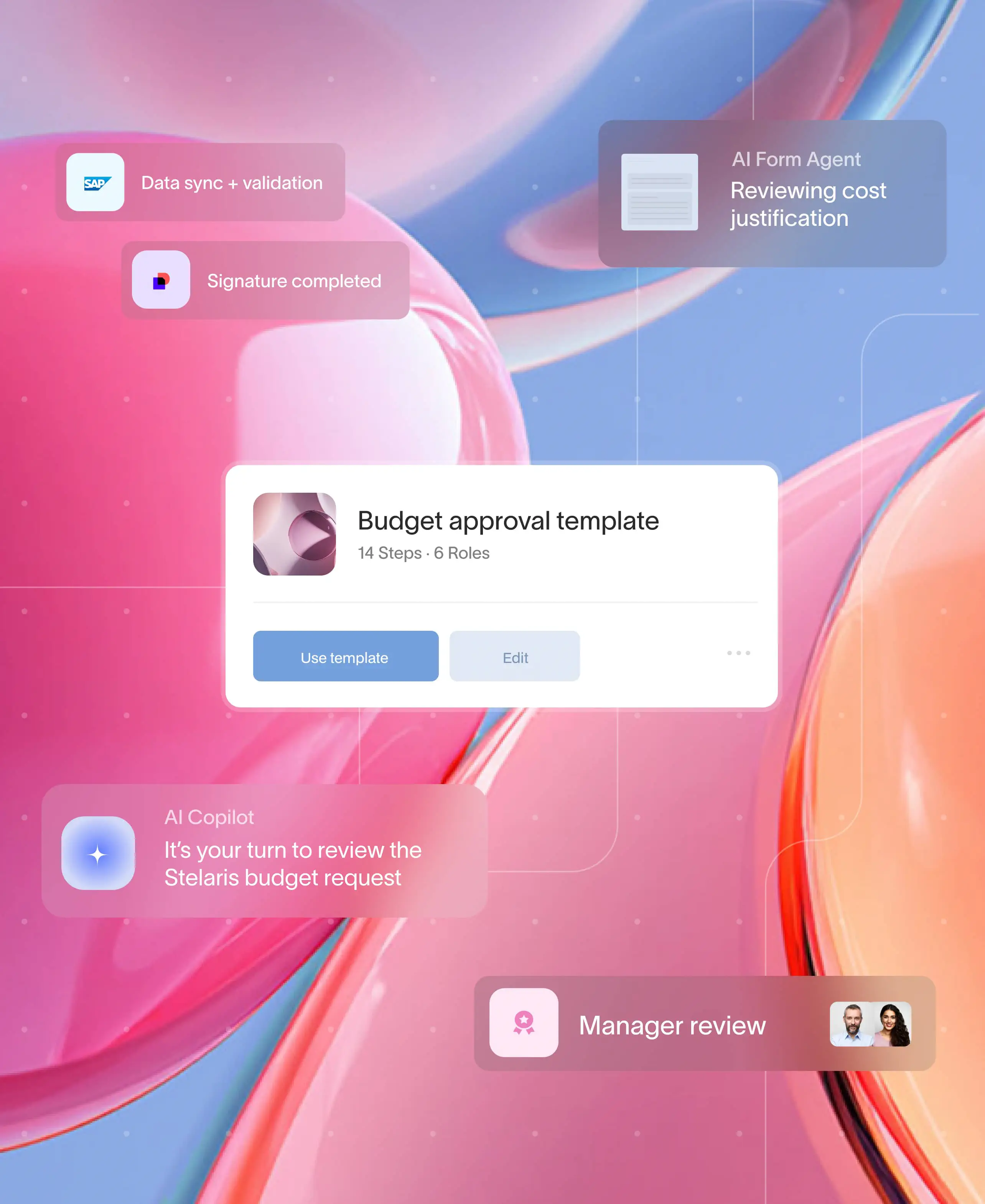
2. Human + AI orchestration
Claims handling requires both empathy and intelligence. Automation software should combine AI-driven efficiencies — like document parsing, fraud detection, and pattern recognition — with human decision points where expert judgment is essential.
3. SLA tracking and escalation logic
Service Level Agreements (SLAs) keep claims accountable. Look for systems that allow custom SLA timers, reminders, and automated escalations when deadlines are missed — ensuring no claim stalls or goes dark.
4. Seamless external collaboration
A strong claims automation solution should connect internal teams with policyholders, brokers, and vendors in one secure environment. Features like client portals, document-sharing links, and chat-based task threads create transparency without compromising security.
5. Built-in compliance and audit trails
Insurance operations live and die by documentation. The right tool will automatically log every comment, approval, and file upload, maintaining traceability for audits and regulatory reviews — without adding admin overhead.
6. Integration with existing core systems
Your automation platform should complement, not replace, your core claims management or policy systems. Prioritize solutions that integrate seamlessly through APIs, webhooks, or data connectors, ensuring your tech ecosystem stays unified.
7. Customization and scalability
No two insurers operate the same way. The right solution offers no-code configurability, letting teams tailor workflows and forms without relying on IT. It should also scale effortlessly across departments, product lines, and geographies.
8. Modern, branded user experience
Finally, great claims automation isn’t just back-end efficient — it’s front-end intuitive. A modern, branded, client-facing interface helps create trust and consistency, turning operational excellence into a customer experience advantage.
How Moxo delivers
When evaluating claims automation software, the goal isn’t just speed — it’s orchestration. The right platform should unify people, systems, and AI under one seamless experience. Here’s what to look for — and how Moxo delivers on each front:
In short: Moxo isn’t just a claims automation platform — it’s an orchestration layer that brings human, system, and AI-driven steps together in one cohesive flow.
Evaluation criteria for choosing the right claims automation software
Even the most advanced platforms can fall short if they don’t align with your organization’s needs. Use these criteria to evaluate which solution fits best.
1. Integration and interoperability
Your automation system should fit into your existing tech stack, not fight it. Evaluate how easily it connects with your core claims management system, CRM, ERP, and document repositories. Look for open APIs, pre-built connectors, and strong data security protocols.
2. Ease of use and configurability
A powerful tool that requires IT to build every workflow isn’t scalable. Choose software that allows no-code or low-code customization, enabling operations teams to design and modify workflows without technical dependencies.
3. Security and compliance readiness
Insurance processes deal with highly sensitive data. Verify that the vendor complies with SOC 2, ISO 27001, GDPR, and local data-privacy regulations. Built-in encryption, audit logs, and access control should be standard — not optional.
4. Scalability and flexibility
The system must scale across product lines, teams, and geographies as your organization grows. It should support high-volume processing, multilingual environments, and multi-entity configurations without performance loss.
5. Analytics and ROI tracking
Claims automation isn’t complete without visibility into performance. Ensure the solution offers real-time dashboards, KPI tracking, and analytics that help you measure cycle times, SLA adherence, and financial outcomes.
6. Vendor reliability and support
Automation is an evolving journey. Evaluate the vendor’s industry experience, customer support quality, implementation timeline, and roadmap transparency. A good partner grows with your organization, not just sells to it.
Best practices for implementing claims automation
Choosing software is only half the equation — success depends on how you deploy it.
1. Start with high-impact workflows
Begin with one or two bottleneck processes — typically FNOL intake or adjudication reviews — where automation delivers quick wins. Prove ROI early before expanding to the full lifecycle.
2. Involve all stakeholders early
Bring in claims adjusters, compliance officers, IT, and customer experience teams during workflow design. This ensures the solution aligns with real operational needs, not just theoretical ones.
3. Standardize before automating
Automation multiplies whatever exists — good or bad. Establish clear SOPs and decision trees first, then embed them in workflows to ensure consistency.
4. Monitor continuously
Use KPI dashboards to track efficiency, turnaround time, and SLA performance. Review data monthly or quarterly to identify improvement areas.
5. Train and communicate
Even no-code platforms require change management. Provide short, role-specific training sessions and share early success stories to drive adoption.
6. Build for compliance from day one
Integrate evidence capture, version control, and approval checkpoints directly into your workflows to make audits seamless later.
Benefits of adopting claims automation
Modern claims automation doesn’t just digitize processes — it transforms how insurers operate.
1. Faster turnaround times
Automated workflows eliminate redundant hand-offs and manual data entry, reducing claim cycle times by 30–50 % on average.
2. Improved accuracy and consistency
Standardized templates and rule-based decisioning minimize human error and ensure uniform handling across claims and geographies.
3. Greater transparency and control
Every action, comment, and approval is tracked in real time. Managers gain instant visibility into bottlenecks, SLA compliance, and claim status.
4. Enhanced customer experience
Clients benefit from quicker updates, fewer errors, and clear digital communication — boosting satisfaction and retention.
5. Cost efficiency and scalability
By reducing manual effort and paper handling, insurers lower administrative costs while scaling volumes without adding headcount.
6. Built-in compliance and audit readiness
Audit trails, timestamps, and versioned documentation provide regulators with immediate evidence of process integrity.
When chosen and implemented thoughtfully, claims automation becomes more than a workflow upgrade — it’s an operational strategy. It unites people, technology, and insight into one continuous system of efficiency, accountability, and trust.
How Moxo meets the evaluation criteria
Moxo complements, not replaces, your core claims platform — extending it with secure automation, structured workflows, and transparent collaboration. It brings human, system, and AI elements together in one compliant, auditable workspace.
Structured workflows and human checkpoints
Claims depend on precision. With Moxo’s no-code flow builder, insurers can map every checkpoint — from FNOL to approvals — with forms, file requests, and e-signatures. Each step is configurable, trackable, and visible across teams.
AI validation and document intelligence
Moxo’s AI review agents parse documents, extract key data, and validate evidence — reducing rework and giving adjusters cleaner inputs to work with. This shortens cycle times and improves decision quality.
Fraud triage and subrogation workflows
Moxo enables automated triage and referrals for fraud or recovery cases. Suspicious claims are routed to SIU investigators, while subrogation handoffs include evidence packets and structured tasks for faster recovery.
Integrations and collaboration layer
Moxo integrates with existing tools like Jira, Slack, DocuSign, Stripe, Jumio, and payment systems — extending current infrastructure rather than disrupting it. Externally, policyholders, brokers, and vendors collaborate securely via Magic Links — no logins, just real-time visibility and notifications.
Security, compliance, and auditability
Built with enterprise-grade security, Moxo supports SOC 2 and SOC 3 certifications, encryption, and exportable audit trails. SSO and role-based access controls ensure every step remains compliant and traceable.
Reporting and visibility
Executives gain access to real-time dashboards that track leakage, turnaround times, and recovery performance by region, line of business, or adjuster — supporting continuous improvement.
Measurable impact
Organizations using Moxo report:
- 40–60% faster approvals
- 75% more claims handled per adjuster
- 95% less email traffic (based on G2 reviews)
A global financial services firm recently adopted Moxo to unify multi-party claims processing. By digitizing document collection and approvals, they reduced cycle times by 50% while meeting all audit and compliance standards.
In essence: Moxo turns fragmented claims processes into one unified, compliant ecosystem — built for transparency, collaboration, and scale. It doesn’t replace your systems. It enhances them.
Would you invite a policyholder into your claims automation platform? With Moxo, the answer is yes, because it is built as a branded client portal first. Book a demo with Moxo to see how your claims process can be transformed.
Choose what’s right
Choosing the right claims automation software is not about replacing your claims core but about augmenting it with secure, flexible workflows. By focusing on human approvals, AI validation, fraud detection, and reporting, carriers can reduce leakage and improve client satisfaction.
Moxo offers a proven, workflow-first platform that empowers insurers to deliver compliant, efficient claims experiences. Book a demo with Moxo to see how your claims process can be transformed.
FAQs
What is claims automation software?
It is software that orchestrates workflows, documents, and communications across claims stakeholders. With Moxo, insurers get a secure portal that complements their core system.
How does Moxo compare with core claims platforms?
Core platforms manage records. Moxo adds workflow automation, external portals, and audit trails, filling gaps in client-facing processes.
Can claims automation software reduce costs?
Yes. By cutting leakage and improving cycle times, automation can reduce costs by 30% (McKinsey). Moxo clients report faster processing and reduced rework.
Is Moxo secure enough for regulated industries?
Yes. Moxo is SOC 2, SOC 3, GDPR compliant, with encryption, SSO, RBAC, and audit trails for regulator-ready evidence.
What ROI can I expect from claims automation?
With Moxo, insurers typically achieve 40–60% faster approvals, 75% more capacity, and up to 95% less email dependency.