.webp)
At a glance
Connect every stage of the claims lifecycle from FNOL to payment in one visible, auditable workflow.
Automate repetitive validations and communications to reduce manual effort and accelerate claim resolution.
Collaborate securely with stakeholders through shared workspaces and document version control.
Gain real-time insights with built-in dashboards that track cycle time, leakage, and compliance metrics.
What is claims processing
Claims processing is the sequence of steps that transform a reported loss into a verified payout. It includes intake, validation, adjudication, payment, and sometimes recovery. Each phase involves coordination between claimants, adjusters, vendors, and internal teams.
Historically, this coordination has been manual. But as insurers face rising claim volumes and regulatory expectations, many are adopting orchestration platforms like Moxo that unify data, communication, and decision-making. With configurable workflows and audit-ready collaboration, insurers can maintain both speed and control across every case.
The claims processing lifecycle: a sequential view from FNOL to recovery
Stage 1: intake and verification – building data accuracy at first notice of loss (FNOL)
The process begins when a policyholder reports a loss. Data accuracy at this stage determines downstream efficiency. Modern FNOL workflows use structured digital forms, image uploads, and policy verification tools to collect complete data from the start.
Using a digital orchestration solution, FNOL forms can automatically route to the right handler while documents are securely stored in a centralized client portal. Automated validation ensures data accuracy and completeness, preventing rework later in the process.
Stage 2: triage and routing – prioritizing claims using rule-based logic
Once intake is complete, the claim must be categorized by severity and complexity. Rule-based routing ensures that high-value or high-risk claims receive additional oversight while simpler claims move through straight-through processing.
Through Moxo’s Flow Builder, teams can configure branching logic, thresholds, and SLAs that prioritize urgent cases and prevent bottlenecks. Every action is time-stamped, giving leaders real-time visibility into progress.
Stage 3: adjudication and approvals – where human judgment meets automation
Adjudication is the decision-making heart of claims processing. Adjusters assess liability, verify coverage, and determine payouts. Automation assists by checking document completeness and applying rules, while humans handle exceptions and final approvals.
Inside Moxo’s collaborative workspace, adjusters can annotate documents, leave comments, and complete approvals, all within the same digital thread. This eliminates version confusion and email dependency while maintaining a full audit trail.
Stage 4: payment and closeout – ensuring traceable disbursements
Once approved, the claim transitions to payment. Integration with accounting and payment systems enables disbursements with full traceability. Notifications are automated so claimants and vendors stay informed.
Every approval, transfer, and message is logged automatically, supporting SOC 2 and GDPR compliance while maintaining transparency throughout the payment cycle.
Stage 5: recovery and subrogation – streamlining third-party coordination
When recovery is required from another insurer or third party, shared vendor portals streamline the process. These portals allow partners to upload documentation, track progress, and stay informed on milestones.
This transparency ensures accountability across legal teams, external adjusters, and recovery specialists, minimizing leakage and maintaining clear ownership at every stage.
Tailoring workflows: how orchestration adapts across different claim types
Claims workflows vary across insurance categories, yet the orchestration principles remain constant.
Auto claims rely on quick evidence collection. Document collection tools simplify uploading photos, police reports, and repair estimates for faster resolution.
Property claims demand coordination among assessors, contractors, and finance teams. Shared digital workspaces enable direct communication and centralized tracking.
Health claims require strict confidentiality and regulatory adherence. Moxo’s role-based access and continuous audit trails ensure HIPAA-compliant handling of sensitive data.
Life claims involve verification and documentation from beneficiaries. Integrated eSign workflows reduce turnaround time while maintaining compliance.
Each line of business benefits when stakeholders and systems operate within one unified environment.
Where to apply technology: balancing automation and human oversight
Automation handles repetitive, predictable work, while orchestration ensures every participant, rule, and system operates in sync.
At intake, automated forms validate information and pre-fill policy data. During adjudication, AI tools assist with document verification. In payment and recovery, integration with core systems prevents duplication and errors.
The human-in-the-loop design ensures accuracy where judgment is needed. The result is faster turnaround times and fewer compliance risks – a balance that platforms like Moxo make achievable through connected, configurable workflows.
Orchestration acts like a conductor, ensuring the rhythm of every claim remains smooth, no matter how complex the performance.
Identifying and fixing 4 common claims coordination gaps
Even digital claims systems can struggle with coordination gaps. Typical bottlenecks include:
1. Incomplete FNOL data: Missing fields cause delays. Structured forms and validations capture the right data upfront.
2. Delayed handoffs: Manual follow-ups waste time. Automated notifications within Moxo workflows keep everyone aligned and accountable.
3. Lack of visibility: Without dashboards, it’s difficult to track SLAs. Real-time reporting shows progress and identifies where intervention is needed.
4. Audit gaps: Missing documentation increases risk. Continuous audit logging and exportable records in Moxo simplify compliance reviews.
According to Accenture, a regional insurer that automated status updates and SLA alerts cut its average claim cycle time by 37 percent and reduced reopen rates by one-third.
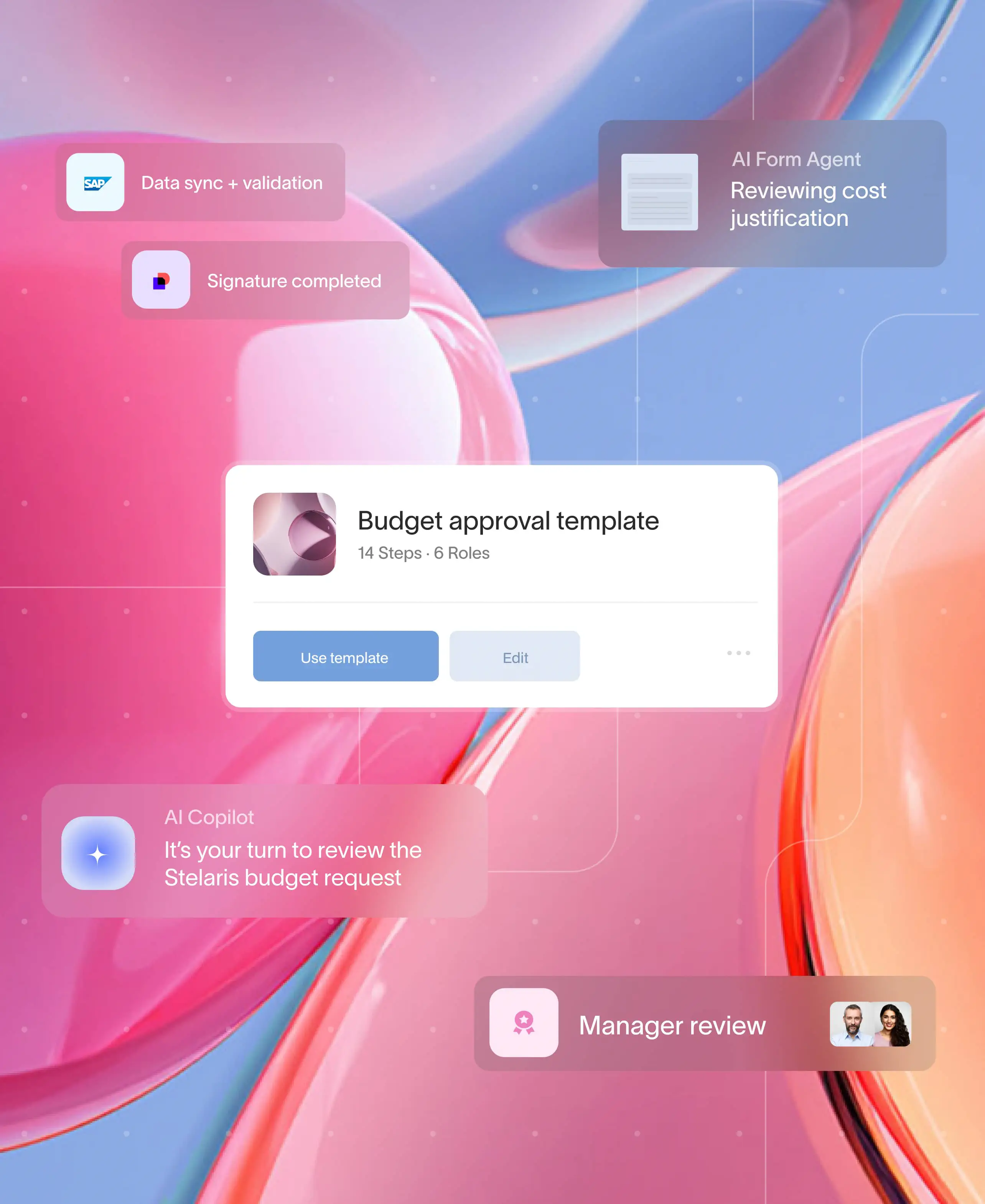
Building your claims workflow in Moxo: Flow builder to final dashboard
Flow builder
Moxo’s visual builder lets teams design FNOL-to-payment flows in minutes using drag-and-drop actions. Intake forms, document requests, and approval steps are added seamlessly to create a unified process.
Controls
Branches, thresholds, and milestones enable real-world flexibility. For example, claims exceeding a certain value can automatically trigger an additional approval layer before payout.
Automations and integrations
With Moxo integrations, workflows can connect directly to policy administration systems, CRMs, or accounting tools. This keeps every dataset synchronized across platforms for consistent records and auditability.
Magic links for externals
Magic links allow external users—policyholders, vendors, or brokers—to complete tasks securely without requiring logins. This reduces friction and ensures faster document submission and approval cycles.
Management reporting
Interactive dashboards display metrics such as cycle time, STP rate, leakage, and re-open rates. Managers can filter by line of business, region, or adjuster to pinpoint performance trends.
Governance and compliance
Moxo includes SSO, MFA, role-based access control, and continuous audit trails. The platform is built with SOC 2 and GDPR compliance in mind, providing enterprise-level security for sensitive insurance data.
Measuring success: key performance indicators (KPIs) for claims excellence
Tracking performance helps insurers move from reactive claims handling to proactive improvement.
Cycle time: Measures how long it takes to close a claim from FNOL to payout.
Straight-through processing (STP) rate: Calculates claims handled without manual intervention.
Severity: Tracks average payout size to identify high-cost trends.
Leakage: Highlights preventable losses from errors or inefficiencies.
A Deloitte study found that insurers using advanced analytics and orchestration improved claim cycle times by more than 20 percent within six months.
Templates and next steps
Modernizing claims doesn’t require a full rebuild. Start with Moxo’s in-built ready-to-go templates.
Moxo’s claims processing template bundle includes pre-configured FNOL intake flows, adjudication paths, payment subflows, and performance dashboards. Each can be adapted by business line, geography, or policy type.
To explore these capabilities further, learn more about workflows, document collection, client portal, vendor portal, and security in Moxo.
Traditional vs orchestrated claims processing
From complexity to clarity: the future of claims management
Streamlining claims processing is not only about speed; it is about clarity, accountability, and consistency across every touchpoint. When insurers connect intake, adjudication, and payment within a single, transparent workflow, they gain the visibility to manage exceptions quickly and the data to make smarter decisions. This level of control turns a historically reactive process into a predictable, value-driven operation.
Moxo strengthens that foundation with practical orchestration tools. Its no-code workflow builder, automated routing, and secure collaboration spaces help teams design and manage end-to-end claims journeys without toggling between systems. With real-time updates, integrated approvals, and full audit trails, it keeps every participant aligned while maintaining compliance with SOC 2 and GDPR standards.
Looking to modernize your claims operations? Explore how Moxo turns complex claim handling into a connected, transparent experience — schedule a demo to see it in action.
FAQs
What is claims processing in insurance
Claims processing is the structured workflow where an insurer receives, verifies, and settles a policyholder’s claim for loss or damage. It includes stages like FNOL, adjudication, payment, and recovery.
How can automation improve claims processing
Automation handles repetitive tasks such as form validation and data checks. When combined with orchestration platforms like Moxo, it ensures every claim progresses seamlessly from intake to settlement without manual bottlenecks.
What are the main stages of claims processing
The lifecycle includes FNOL (intake), triage, adjudication, payment, and recovery or subrogation. Each phase relies on clear communication and documentation between internal and external stakeholders.
What KPIs should teams track for claims performance
Key metrics include cycle time, straight-through processing rate, claim severity, and leakage percentage. Moxo dashboards visualize these metrics in real time for faster decision-making.
How does Moxo ensure data security and compliance
Moxo operates with enterprise-grade standards such as SOC 2 and GDPR compliance. It offers role-based access control, multifactor authentication, and continuous audit trails to protect sensitive claim data.