At a glance
Modern healthcare claims processing requires speed, accuracy, and compliance across payers, providers, and clearinghouses.
By connecting every submission, validation, and appeal into a single workflow, teams minimize rework and delays.
With AI-assisted coding, EDI automation (837/835), and real-time collaboration, healthcare organizations achieve faster reimbursements and lower denial rates.
Moxo enables HIPAA-compliant orchestration that keeps patient data secure while simplifying every claims step from intake to audit.
What is a claims processing software for healthcare?
Healthcare claims processing software automates how claims are created, validated, adjudicated, and reimbursed between providers and payers.
It manages electronic data interchange (EDI), verifies codes, captures documentation, and ensures compliance with HIPAA and SOC 2 security standards.
Traditional systems handle claim transactions but often lack the workflow coordination needed between people — the billing staff, coders, and payers who must collaborate on corrections or appeals.
Moxo’s workflow orchestration platform fills that gap by connecting human review, documentation, and system integrations in one secure workspace.
Every task, document, and EDI handoff is tracked, creating an audit-ready claims process from submission to payment.
Why you need a healthcare claims processing software: automating the 4 stages
The complexity of healthcare reimbursement from coding validation to payment reconciliation makes manual coordination nearly impossible.
A robust claims processing platform helps reduce denials, ensure PHI security, and improve financial transparency across the revenue cycle.
Let’s break down the major stages and how modern software supports each one.
Stage 1: secure intake and documentation with HIPAA-compliant automation
The claims journey begins with accurate intake.
Providers submit encounter data, charge sheets, and supporting documents that must be validated before submission to payers.
Moxo simplifies this through intake workflows that:
- Capture forms and supporting documentation through secure upload requests
- Apply AI-based validation to confirm required data fields are complete
- Maintain encryption at rest and in transit, ensuring HIPAA and PHI compliance
Example:
A healthcare billing firm implemented digital intake forms and automated document checks, reducing missing-data rejections by 42% within the first quarter.
Stage 2: improving coding accuracy with AI-assisted validation
Accurate coding is critical for payer acceptance—incorrect CPT or ICD-10 codes can lead to denials or delays.
Moxo supports coding accuracy by reviewing claims for code consistency, flagging mismatched diagnosis-procedure pairs, and identifying missing modifiers based on historical data.
With built-in validation and audit tracking, coding teams can correct errors before EDI submission, ensuring compliance and accelerating reimbursement.
Stage 3: streamlining adjudication follow-up and appeals coordination
Once claims are submitted via EDI 837 transactions, payers process them for adjudication.
Rejections or partial payments often trigger a manual appeal, which involves document exchange and justification from the provider side.
Moxo orchestrates this back-and-forth through secure, traceable collaboration.
Payers and providers can exchange documents through Magic Links, keeping PHI encrypted while maintaining full audit visibility.
Example:
A large multi-specialty provider used Moxo to manage EDI submission follow-ups and appeals, tracking all documentation and approvals within the same workflow.
The outcome: Denials reduced by 36% and appeal turnaround improved by 28%, as cited in their case study.
Stage 4: linking remits and payments for accurate reconciliation
After adjudication, payments and remittance advice (EDI 835) flow back to providers.
Reconciling these transactions with the original submissions requires accuracy and traceability.
Through Moxo Integrations with billing and accounting systems, remits are automatically linked to the corresponding claims. Finance teams gain visibility into status updates, explanations of benefits, and remaining balances, all in one view.
Every EDI file, note, and communication remains secured under Moxo’s security controls, ensuring full HIPAA and SOC 2 alignment.
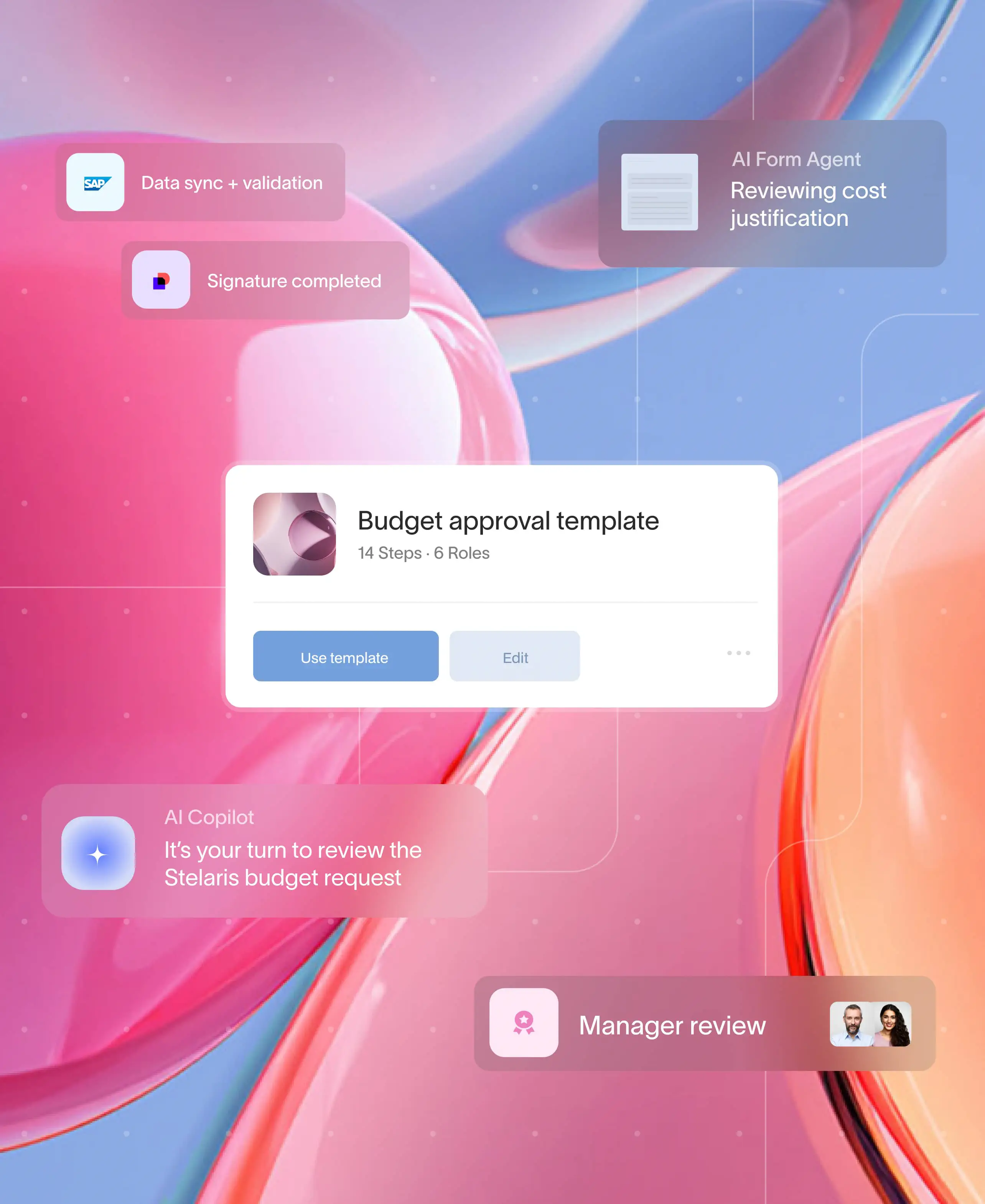
Building your compliant healthcare claims workflow in Moxo
Flow builder (intake forms, file requests, approvals, eSign)
Start by modeling your claims workflow using Moxo Flow Builder.
Create digital intake forms for claim submissions, add approval steps for coding validation, and capture eSignatures for audit evidence.
Every document is stored securely and traceable to the specific claim record.
Controls (branches, thresholds, SLAs, milestones)
Use conditional branches and SLA milestones to route claims automatically.
For instance, claims over a defined threshold or with flagged codes can be routed to senior billing specialists for review.
Automated SLAs ensure no claim remains idle beyond payer submission timelines.
Automations & integrations (policy / claims core, CRM, DMS, payments, eSign / ID)
Through Moxo integrations, connect EHR, billing, and accounting systems to synchronize claim status and payment data.
Moxo supports REST APIs, event-based triggers, and secure file transfers that align with healthcare’s interoperability standards.
This integration also supports EDI workflows (837 submission and 835 reconciliation), creating a continuous data loop between systems.
Magic links for externals (providers, clearinghouses, payers)
Replace unsecured emails with Magic Links that grant external partners secure, one-click access to their assigned tasks.
Providers, clearinghouses, and payers can exchange forms, remittance details, or documentation safely without managing multiple portals.
Management reporting (cycle time, denial rate, payment lag, appeal volume)
Moxo’s analytics dashboard combines workflow and financial data to deliver metrics like average reimbursement time, denial rate, and appeal success.
Leaders can segment these KPIs by payer, specialty, or location to uncover trends and optimize resource allocation.
Governance (SSO/SAML, RBAC, HIPAA/PHI handling, audit trails & export)
Compliance sits at the heart of healthcare claims operations.
Moxo offers SOC 2 and HIPAA-aligned governance controls, including SSO/SAML authentication, MFA, role-based access, and PHI encryption.
Every claim activity, approval, and document exchange is logged with metadata for audit purposes, and audit exports can be generated on demand.
Real-world example: healthcare claims efficiency at scale
A healthcare third-party administrator used Moxo to centralize payer-provider communication and automate intake documentation.
Through integrations with its EHR and billing systems, Moxo orchestrated intake validation, appeals, and remittance reconciliation under one secure workflow.
Results within 6 months:
- Denial rate reduced by 40 %
- PHI access audit time cut from 2 weeks to 3 days
- Staff productivity increased by 30 %
This outcome demonstrated how orchestration — not just automation — drives measurable ROI in healthcare claims management.
How Moxo helps
Healthcare claims need speed, accuracy, and HIPAA compliance. Moxo automates claim intake, document validation, and multi-party collaboration – securely and transparently.
With workflow automation, claims route automatically to reviewers based on policy type or dollar value. Document workflows manage PHI with encryption and access controls that meet HIPAA and SOC 2 standards.
Providers and insurers collaborate in branded client portals, while performance dashboards monitor cycle time, denial rate, and SLA compliance.
Moxo simplifies healthcare claims, keeping data protected and decisions traceable from submission to payout.
Secure orchestration, smarter healthcare claims
Healthcare claims processing is about more than transactions; it is about trust and accuracy.
By connecting intake, coding, adjudication, and reconciliation into a unified workflow, providers and payers gain full visibility while protecting PHI.
When every claim is tracked, validated, and audited automatically, compliance becomes effortless.
That is where Moxo enhances the process. Its no-code orchestration platform connects people, documents, and systems into a secure, HIPAA-compliant environment.
With real-time collaboration, built-in AI validation, and EDI integration capabilities, healthcare organizations can accelerate reimbursements while maintaining complete control of sensitive data.
Ready to simplify your healthcare claims workflows? Explore how Moxo turns complexity into clarity: Schedule a demo to see it in action.
FAQs
What is healthcare claims processing software?
It is a system that automates how claims move from provider to payer, managing validation, adjudication, and payment. Moxo extends this process through secure, HIPAA-compliant orchestration that connects every participant.
How does Moxo support EDI 837 and 835 workflows?
Through Moxo Integrations, organizations can synchronize submission (837) and remittance (835) data, linking them to task-based workflows and financial reporting dashboards.
Can Moxo handle PHI and HIPAA compliance?
Yes. Moxo Security enforces SOC 2 and HIPAA standards with encryption, MFA, audit trails, and role-based access controls.
Does Moxo integrate with EHR or billing systems?
Yes. Moxo’s API framework connects with EHR platforms, billing software, and clearinghouses for seamless data flow.
What ROI can healthcare teams expect?
Organizations featured in Moxo’s customer stories achieved faster claims turnaround, lower denial rates, and improved audit readiness through intelligent orchestration.