At a glance
Policyholders expect transparency, trust, and speed—not just a payout—when filing a claim.
Claims status portals provide real-time updates, document sharing, and visibility into every decision.
For insurers, this means faster cycle times, higher satisfaction, and fewer disputes.
Moxo modernizes communication with secure Magic Links, automated workflows, and reporting dashboards for a seamless client experience.
Revolutionizing the policyholder experience
In today's fast-paced world, policyholders expect seamless, transparent, and immediate access to information, especially when it comes to their insurance claims. Modern claims status and communication portals are no longer just a convenience; they are a critical component for enhancing client experience and building trust. These innovative platforms empower insurers to keep policyholders informed at every stage of their claim, transforming what can often be a stressful process into a smooth and reassuring journey.
The claims experience gap
Insurance claims are often described as the moment of truth for customers. It’s a time when policyholders expect fast, clear, and reliable communication. Yet, despite significant investments in digital tools, many carriers still fall short, particularly after the first notice of loss (FNOL). According to J.D. Power’s 2023 U.S. Property Claims Satisfaction Study, policyholder satisfaction has declined, with a lack of status updates cited as a key driver. Customers continue to ask the same question: “What’s happening with my claim?”
This communication gap doesn’t just lead to frustration—it has tangible business consequences. Miscommunication or poor status updates can result in disputes, erode trust, reduce loyalty, and ultimately cause insurers to lose customers. In an industry where competition is fierce, no company can afford these outcomes.
A modern claims status portal is no longer optional—it’s an essential tool for delivering a transparent and seamless claims journey. Such portals can provide:
- Real-time updates: Give customers visibility into every step of the claims process, easing their concerns and reducing the need for follow-ups.
- Customizable notifications: Keep policyholders informed via email, SMS, or app notifications, allowing them to choose their preferred communication channels.
- Self-service options: Empower customers to upload documents, view claim status, and ask questions at their convenience.
- Two-way communication: Create opportunities for customers to ask questions and get personalized responses quickly, improving engagement and trust.
- Analytics for insurers: Track customer interactions and identify potential bottlenecks in the claims process to refine operations.
By adopting a modern claims status and communication platform, insurers can bridge the communication gap, enhance the customer experience, and foster long-term loyalty, turning the "moment of truth" into an opportunity to build stronger relationships.
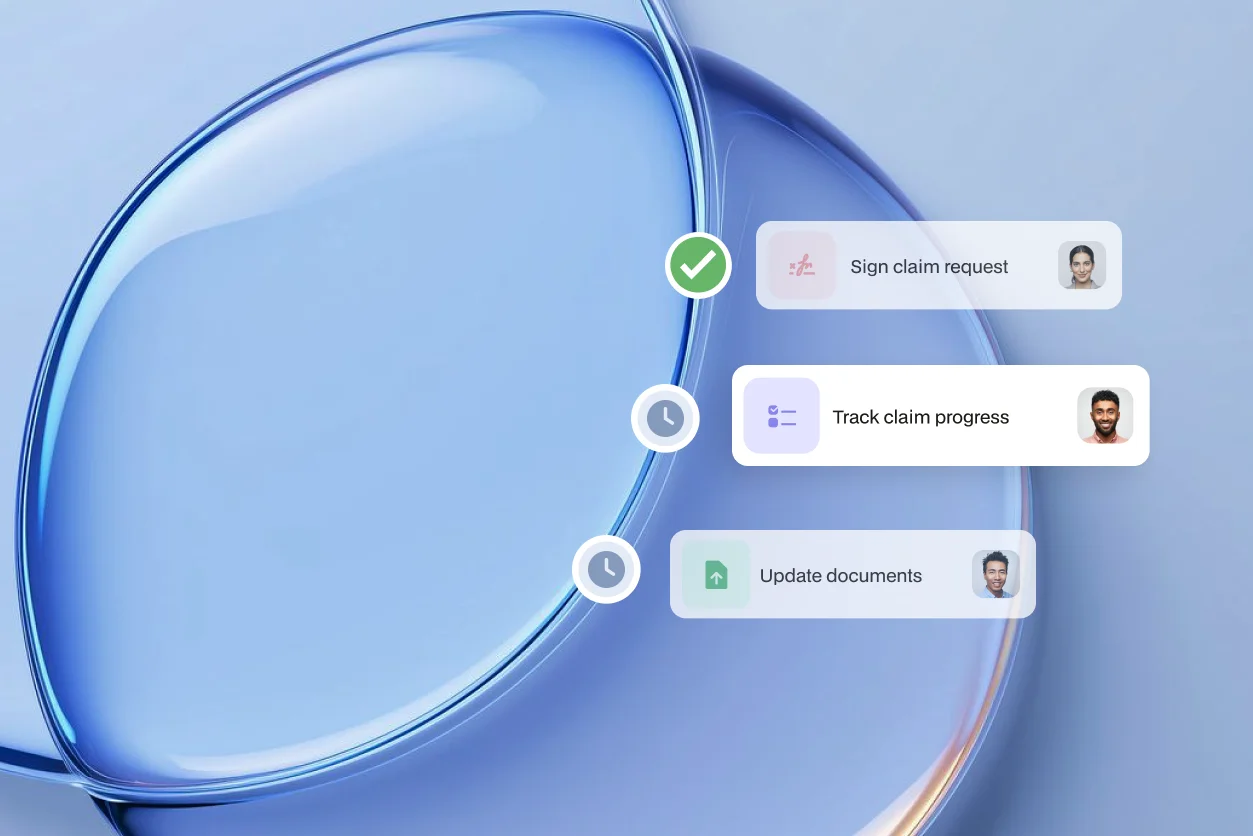
What policyholders need to see to stay informed and reassured
When a claim arises, policyholders seek reassurance and clarity, not uncertainty. A modern claims status and communication portal is essential for delivering an exceptional client experience by keeping them updated at every step. Such a portal should provide:
Real-time claim status: Showing crucial milestones like FNOL received, adjuster assigned, and settlement issued. This immediate visibility dramatically reduces anxiety and keeps policyholders feeling in control, knowing exactly where their claim stands without having to constantly call.
Secure document upload and access: Allowing policyholders to easily submit required documents and securely access their own claim-related paperwork. This eliminates email backlogs, misplaced attachments, and provides a single, reliable source for all important files.
Evidence and decision transparency: Policyholders need to see the “why” behind outcomes. Providing clear explanations and supporting evidence fosters trust, ensuring they understand the rationale behind decisions rather than feeling confused or dismissed.
Direct communication channels: Beyond just status updates, a robust portal offers intuitive ways to communicate directly with adjusters or support teams. This ensures specific questions are answered promptly and efficiently, reducing frustration.
Dispute channels with clear SLAs: Offering accessible pathways for raising concerns or disputing decisions, backed by service level agreements, demonstrates a commitment to fair resolution and accountability.
Research by McKinsey highlights that transparency and automation in claims can boost retention by up to 30%. This directly translates to faster, more efficient service and happier policyholders.
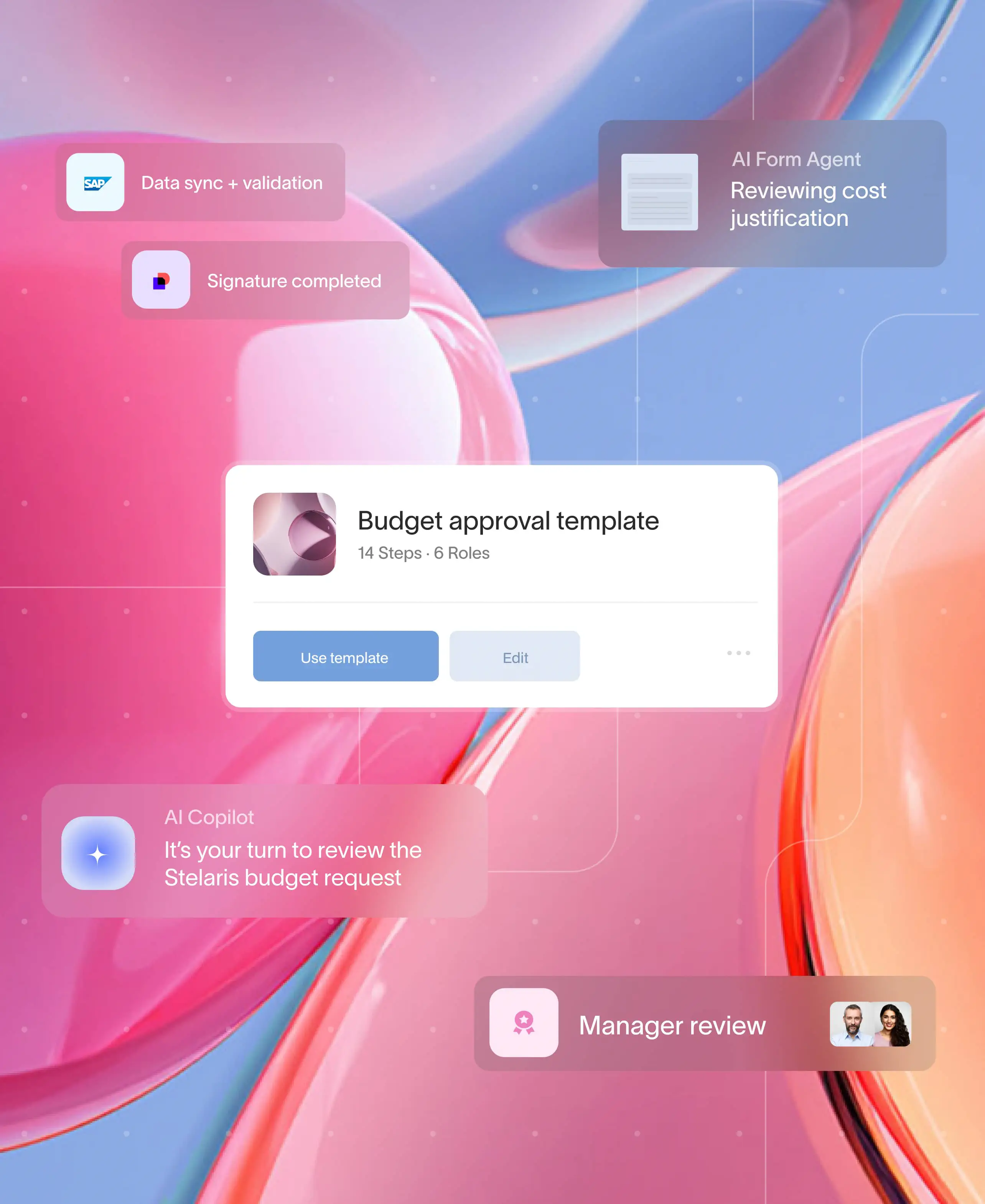
Build the portal in Moxo with Magic Links
The challenge: Keeping policyholders informed and engaged
One of the biggest frustrations for policyholders is the lack of real-time updates and seamless communication during the claims process. Traditional methods often leave them in the dark, leading to calls, emails, and a poor overall experience. A dedicated claims portal is the answer, but often, the biggest barrier to its success is adoption. Traditional platforms demand logins, app downloads, and password resets – all friction points that discourage use and prevent policyholders from staying updated.
The solution: Instant access for a superior client experience
Moxo eliminates this friction with Magic Links — secure, single-use links that open the claims workspace instantly. Imagine a policyholder receiving a notification and being able to access their claim status, upload documents, or communicate with their adjuster in seconds, without remembering a single password.
Whether on desktop or mobile, policyholders, brokers, and third-party vendors can join seamlessly, without IT overhead. This instant access means:
Policyholders stay informed: They get real-time updates on their claim's progress at every step, reducing anxiety and phone calls.
Improved transparency: All parties have a clear, shared view of the claims journey.
Enhanced collaboration: Brokers and vendors can contribute efficiently, speeding up resolution.
By combining this with mobile-first design and a branded client portal, Moxo ensures insurers deliver critical transparency and efficient communication, all while protecting sensitive data with enterprise-grade security and compliance. This builds trust and significantly improves the client experience from first notice of loss to final settlement.
Status, evidence & disputes
A successful claims portal must be more than just a static tracker; it needs to be the single source of truth for the entire claims lifecycle. This transparency is crucial for building and maintaining policyholder trust. Moxo enables insurers to provide this level of detail by allowing them to:
Share milestone-based status updates: Proactively inform customers of progress as their claim moves through each stage, from initial submission to final resolution. This eliminates the need for customers to call for updates and reduces anxiety.
Attach and centralize all relevant documents: Securely upload and store photos, reports, and other evidence directly within the claim file, ensuring all parties have access to the same information for complete transparency.
Provide clear decision rationales: When a decision is made, insurers can clearly explain the reasoning behind approvals or denials, attaching supporting evidence directly.
Route disputes into structured workflows: If a customer disputes a decision, the portal can initiate a structured workflow with clear steps, assigned personnel, and complete audit trails for compliance and fair resolution.
Even in the case of a denied claim, providing clear evidence and a well-explained rationale helps preserve the customer relationship and maintain trust—far more effectively than a cryptic, impersonal rejection email ever could. This transparent approach demonstrates fairness and can prevent future disputes.
Reporting & NPS Targets
Insurers can’t improve what they can’t measure. A modern claims status portal should double as a robust management reporting tool, providing real-time data and insights to leadership. By tracking key performance indicators (KPIs), insurers can identify bottlenecks, optimize processes, and ultimately enhance the policyholder experience.
Essential metrics to track include:
Average cycle times: Monitor the duration from claim filing to settlement, broken down by line of business, claim type, or even individual adjuster. This helps pinpoint delays and areas for process improvement.
Straight-through processing (STP) rate: Measure the percentage of claims that are handled automatically without human intervention. A higher STP rate indicates greater efficiency and lower operational costs.
Dispute frequency and resolution time: Track how often claims are disputed and how long it takes to resolve them. High dispute rates may signal issues with clarity in communication or policy terms.
Claim re-open rates and leakage: Monitor how frequently settled claims are re-opened and identify any unnecessary payouts (leakage). These metrics are crucial for assessing claims handling accuracy and financial control.
Policyholder Net Promoter Score (NPS): Continuously gauge customer satisfaction by collecting feedback at key milestones in the claims process. Segmenting NPS by channel, region, or claim complexity can reveal specific strengths and weaknesses in your service delivery.
For example, a consulting client using Moxo reduced cycle time by 35% after automating evidence collection. With access to real-time dashboards, leadership identified process bottlenecks and could dynamically reallocate adjusters to where they were needed most, improving both operational efficiency and customer satisfaction. This data-driven approach transforms the claims portal from a simple communication tool into a strategic asset for continuous improvement.
Build it in Moxo (step by step)
Moxo goes beyond simple intake to create a connected, automated, and compliant claims experience that benefits both insurers and policyholders. It streamlines every stage of the process — from first notice of loss to settlement — while maintaining full visibility, accountability, and control.
Multi-channel claims intake
Enable customers to submit claims through web, mobile, or in-app channels using branded client portals. Moxo supports instant ID and policy verification, so intake is faster, more accurate, and fully traceable.
Automated triage and assignment
Use workflow automation to intelligently route each claim to the right adjuster based on policy type, claim value, or SLA thresholds. Built-in automations handle escalations, reminders, and status updates — minimizing manual intervention.
Secure client-facing collaboration
Replace fragmented emails with a single, branded space for evidence sharing, document exchange, and task tracking. External participants like policyholders, brokers, or vendors can join via magic links — no login or training required.
Dashboards and compliance reporting
Gain real-time visibility into claim cycle times, leakage prevention, and adjuster performance through performance dashboards. Leadership teams can track KPIs, segment by region or product, and export reports for audits in a few clicks.
Enterprise-grade security
Moxo is built with SOC 2 and SOC 3 certification, encryption, and HIPAA/PHI readiness. Every file, message, and decision is logged through immutable audit trails, ensuring regulatory compliance and data integrity.
Proven impact
A regional insurer using Moxo reported a 54% reduction in claim cycle times and measurable improvement in customer retention after digitizing document collection and automating approvals.
Comparison & decision factors
Would you invite a client into a static, internal-only tool? Most carriers wouldn’t. Moxo’s portal is purpose-built for multi-party orchestration, uniting policyholders, brokers, and providers in one secure experience.
How Moxo helps
Moxo simplifies catastrophe claims management by turning surge chaos into structured collaboration. Claims teams, brokers, and vendors work inside one secure portal instead of juggling emails or shared drives.
Streamlined intake: Policyholders submit FNOLs through branded portals with guided forms, file uploads, and digital acknowledgments.
Automated routing: Every claim moves automatically to the right adjuster or manager based on severity, region, or claim type.
Integrated communication: Magic Links and notifications keep external parties informed in real time without requiring logins.
SLA tracking: Built-in milestones, reminders, and dashboards give leaders visibility into turnaround times and compliance.
Audit-ready visibility: All messages, files, and approvals are automatically logged for regulatory review.
By centralizing intake, routing, and communications, Moxo allows insurers to handle CAT surges with speed, accountability, and clarity, without disrupting their existing claims systems.
The bottom line: Turning catastrophe claims into controlled workflows
Catastrophe claims don't have to lead to operational chaos. During surge events, insurers require a streamlined process that includes fast intake, transparent routing, and instant communication with all stakeholders. Using separate tools for each part of this process can create inconsistencies and inefficiencies. Policyholders desire transparency, insurers aim for efficiency, and regulators demand accountability. A centralized claims status portal can meet all three of these needs, ensuring a smoother experience for everyone involved.
Moxo bridges the gap with a workflow-first approach that unites claimants, brokers, vendors, and internal teams in one compliant, secure workspace. The result is faster response times, clearer accountability, and higher client satisfaction, all while reducing manual effort and email overload.
With surge-ready templates, automated SLAs, and real-time dashboards, Moxo helps insurers move from firefighting to foresight. The next time disaster strikes, your claims process can stay calm, coordinated, and in control.
Don’t let outdated claims communication slow you down — get started with Moxo today.
FAQs
What is a claims status portal?
A claims status portal is a secure space where policyholders can track claims, upload documents, and receive real-time updates. With Moxo, this is delivered through branded, mobile-first portals.
How does a claims portal reduce disputes?
By linking evidence, decisions, and audit trails to every claim, disputes are minimized. Moxo automates escalations and SLAs, ensuring fair and timely resolution.
What ROI can insurers expect from claims portals?
Insurers report 40–60% faster approvals, 95% fewer emails, and higher NPS. Moxo clients also gain adjuster efficiency and measurable cycle time reductions.
How is Moxo different from legacy portals?
Legacy portals are static and internal-only. Moxo uses Magic Links for adoption, integrates with claims systems, and ensures compliance, all in one workflow-first portal.
Can Moxo integrate with existing claims systems?
Yes. Moxo connects with claims cores, CRMs, payments, and ID verification tools. It complements existing systems rather than replacing them.