At a glance
The first notice of loss (FNOL) marks the true start of every insurance claim and heavily influences customer trust.
Efficient intake across web, SMS, phone, or email ensures accurate evidence capture and quick policy verification.
Severity scoring, adjuster assignment, and clear communication standards define how fast and confidently claims progress.
Moxo streamlines FNOL workflows with automation, structured collaboration, and real-time visibility to reduce leakage and speed resolutions.
Streamlining the FNOL process: From intake to triage
The First Notice of Loss (FNOL) is a critical step in the insurance claims process, often setting the tone for the entire customer experience. A seamless and efficient FNOL workflow ensures that claims are handled quickly and accurately, minimizing delays and improving customer satisfaction. By optimizing the intake and triage process, insurers can not only enhance operational efficiency but also build trust with their customers when they need it most. This section explores how to streamline the FNOL process for better outcomes.
Why the FNOL workflow matters
When a policyholder files a claim, the clock starts ticking. The efficiency and accuracy of the First Notice of Loss (FNOL) process are critical, setting the tone for the entire claims journey. Research shows that a staggering 60% of claims lifecycle costs are directly influenced by decisions made and data collected during this initial FNOL stage. Despite this, many insurers continue to rely on antiquated methods, such as handwritten notes from phone calls, disorganized email inboxes overflowing with attachments, or disjointed legacy systems that don't communicate effectively.
This inefficiency creates a cascade of problems:
Unnecessary delays: Manual data entry, re-keying information, and searching through disparate sources slow down processing time significantly.
Increased claims leakage: Incomplete or inaccurate information collected at FNOL can lead to poor decisions later, resulting in overpayments or missed subrogation opportunities.
Frustrated customers: Policyholders are often in stressful situations when filing a claim. A cumbersome or slow FNOL process exacerbates their anxiety and negatively impacts their experience and loyalty.
Compliance risks: Inconsistent data capture and lack of audit trails can make it difficult to meet regulatory requirements and demonstrate compliance.
A structured and optimized FNOL workflow eliminates these pain points. By standardizing the intake process, insurers can efficiently manage critical first steps: verify identity and policy details accurately, capture essential evidence (like photos or initial descriptions of damage) effectively, and triage cases quickly to the right adjusters or specialized teams. All of this can be achieved while maintaining strict compliance standards and ensuring transparency for both the insurer and the policyholder, setting the stage for a smooth, cost-effective, and customer-centric claims experience.
Intake channels and verification: The gateway to an efficient FNOL workflow
A modern First Notice of Loss (FNOL) workflow begins with accessible and diverse intake channels, recognizing that policyholders expect choice and convenience when reporting a loss. Providing multiple entry points not only enhances the customer experience but also sets the stage for efficient data capture and subsequent triage.
A robust FNOL system should seamlessly accommodate:
Phone or call centers: Still a primary channel, especially for complex claims, older demographics, or emergency situations. While traditionally resource-intensive, integrating call data with digital systems is crucial for streamlining.
SMS and messaging apps: Ideal for quick, brief notifications and rapid photo/video submissions. These channels can significantly reduce initial reporting time and provide immediate visual evidence.
Email: Offers a convenient, asynchronous option for policyholders to provide detailed information. However, without structured workflows, email submissions can be time-intensive for insurers to process, often requiring manual data extraction.
Web portals and mobile-first apps: These digital channels are increasingly vital. They allow insurers to guide users through structured forms, ensuring accurate and complete data capture from the outset. This "clean data" is invaluable for automated processing and faster triage. They also empower policyholders with self-service capabilities.
API integrations (e.g., IoT, smart home devices): For a truly modern FNOL, consider direct data feeds from connected devices that can automatically detect and report incidents, accelerating the FNOL process significantly (e.g., vehicle telematics after an accident).
Once the initial intake occurs, identity verification is the critical next step. This can range from a simple policy lookup using provided details to more advanced solutions like AI-powered ID scanning tools (e.g., Jumio, Onfido). Streamlining verification with secure and efficient processes offers multiple benefits: it drastically reduces fraud risk, prevents repetitive questions that can frustrate policyholders and erode trust, and speeds up the entire claims journey. By making intake and verification seamless, insurers lay the foundation for a truly efficient FNOL workflow that benefits both the policyholder and the organization.
Evidence capture: Photos, statements and beyond
One of the most critical components of an effective FNOL workflow is the ability to capture comprehensive and accurate evidence right from the start. This immediate intake of crucial information is paramount for seamless processing and efficient triage, ultimately leading to faster resolution.
Imagine a customer reporting hail damage to their car. Instead of waiting for an assessor, they can immediately snap photos on their phone, upload them directly to your secure FNOL portal, and record a brief audio statement detailing the incident. This real-time, digital capture prevents disputes, reduces back-and-forth communication, and lays the groundwork for faster, more accurate claims processing from day one.
Strong FNOL workflows empower claimants to provide vital information effortlessly, encouraging:
Geo-tagged photos and videos: Critical visual proof with embedded timestamps and locations, ensuring authenticity and context.
Immediate voice or text statements: Allowing claimants to quickly document their perspective and the sequence of events, which can be invaluable for early assessment.
Seamless submission of third-party evidence: Such as police reports, contractor assessments, or medical records, directly into the system, consolidating all relevant data.
Directly integrating this evidence into a secure, role-based portal doesn't just eliminate endless email chains; it also ensures robust data security and compliance with regulations like SOC 2 and GDPR. This creates an immutable, audit-ready trail, empowering adjusters to make informed decisions faster and expediting the entire claims journey from seamless intake to efficient triage.
Policy and Coverage Checks: The Foundation for Swift Triage
After initial evidence collection, the next critical step in the FNOL workflow is to confirm policy eligibility and coverage. Historically, this involved laborious manual data retrieval from various systems, a process prone to delays and errors.
Today, advanced integrations—often powered by APIs—enable real-time lookups that instantly validate crucial policy details, including:
- Active coverage dates: Ensuring the incident occurred within the policy period.
- Deductibles: Clearly identifying the policyholder's financial responsibility.
- Exclusions: Quickly flagging any specific events or damages not covered.
- Policy limits: Understanding the maximum payout potential.
- Previous claims history: Providing context for potential fraud detection and recurrence.
Why these checks are vital for efficient FNOL
- Reduces adjuster workload: By automating verifications, adjusters can focus on higher-value tasks.
- Accelerates triage: Claims with confirmed coverage can be immediately routed to the appropriate next steps, such as severity scoring or specialized teams.
- Improves accuracy: Real-time data minimizes errors and discrepancies.
- Enhances customer experience: Faster initial confirmation provides peace of mind to policyholders.
- Mitigates fraud risk: Quick access to claims history can flag suspicious patterns early.
For instance, a property damage claim with instantly confirmed active coverage and no relevant exclusions can bypass a manual review queue and be routed directly for severity assessment, significantly speeding up the entire claims journey. This seamless integration ensures claims are handled accurately and efficiently from the very first notice.
Severity scoring and assignment: Automating triage at FNOL
After a customer reports a First Notice of Loss (FNOL), the immediate next step is efficient triage. Not all claims are equal; some can be settled in minutes, while others demand an in-depth investigation. This is where severity scoring and assignment become crucial, allowing insurers to rapidly route cases to the appropriate resources right from the start.
Advanced FNOL systems leverage AI and predefined rules to analyze incoming claim data—such as the type of loss, reported injuries, policy details, and even historical data patterns—to automatically assign a severity score. This intelligent scoring ensures claims are directed correctly, preventing delays and misallocation of resources.
Low-severity claims: Incidents like a cracked windshield or minor property damage can often be fast-tracked for auto-approval or handled by junior adjusters, significantly reducing processing time.
Moderate-severity claims: These might require an adjuster's review but can still move quickly through a streamlined process, perhaps with automated initial communication.
High-severity claims: Complex cases involving significant bodily injury, major property damage, or potential fraud are immediately escalated to specialized teams or senior adjusters, ensuring expert attention from day one.
By automating this critical scoring and assignment during FNOL, insurers can drastically cut cycle times by 40–60%, enhance customer satisfaction, and maintain both fairness and accuracy across their claims operations. It transforms the initial intake into a highly efficient triage system.
Status Communication and SLAs: Building Trust from the First Interaction
The FNOL stage isn't just about collecting information; it's your first opportunity to set clear expectations and build trust with policyholders during a stressful time. After submitting a claim, their immediate questions are often: "Did you get my claim?" and "What happens next?" Providing prompt, transparent communication from the outset is crucial for a seamless intake experience and efficient triage.
Best-in-class FNOL workflows excel by providing:
Real-time status updates via mobile-first portals: allowing policyholders to check their claim status instantly, anytime, anywhere. This reduces inbound calls and enhances convenience.
Automated reminders for missing documents or deadlines: proactively guiding policyholders through the process, preventing delays caused by incomplete information, and ensuring a swift progression to triage. Service-level agreements (SLAs) that define response times: clearly communicating when they can expect to hear back or what the next steps will be, which manages expectations and builds confidence in your efficiency.
Personalized communication channels: offering options like SMS, email, or in-app notifications for updates, catering to policyholder preferences.
According to J.D. Power, proactive communication is one of the top drivers of customer satisfaction in claims. A well-structured FNOL workflow, with robust communication protocols, ensures that no client feels left in the dark, setting the stage for efficient claims processing and a positive customer journey.
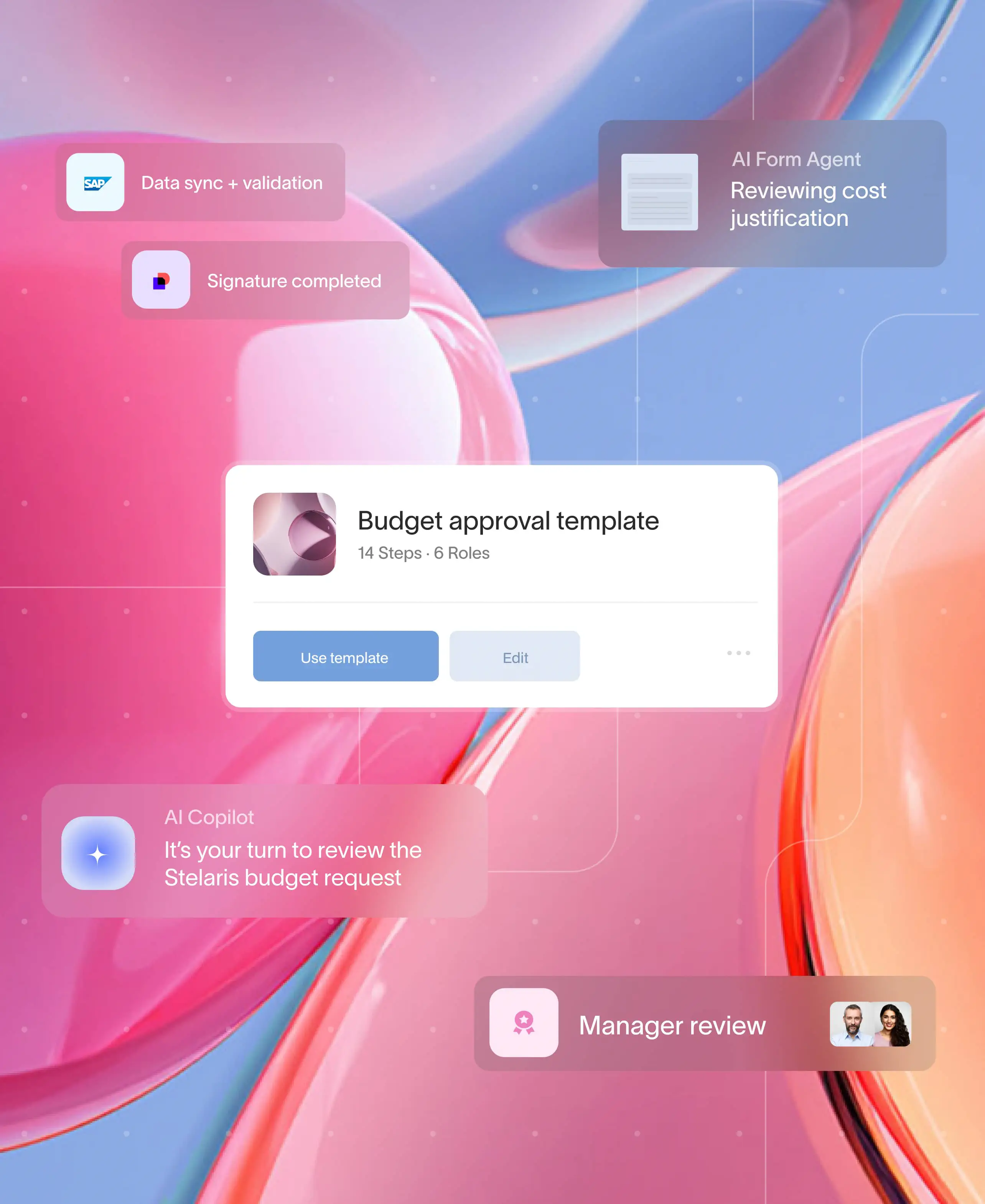
Build it in Moxo: step-by-step
Flow builder
Moxo’s no-code workflow builder lets insurers design FNOL intake processes with drag-and-drop ease. Forms, file requests, approvals, and e-signatures can all be embedded in a single flow.
Controls
Branching logic, milestones, and threshold-based routing help insurers apply severity scoring and SLA controls consistently.
Automations and integrations
With Moxo integrations, FNOL workflows can sync with policy admin systems, CRMs, and even payment rails. Insurers can auto-check coverage, request identity verification, and connect with providers like DocuSign or Jumio.
Magic links for external participants
Policyholders, brokers, or vendors can submit documents via secure magic links without needing a full login—reducing friction while maintaining encryption and audit trails.
AI agents (coming soon)
Moxo is introducing AI agents that review documents, answer claimant questions in real time, and prefill forms based on submitted evidence.
Management reporting
Executives can access dashboards on Moxo’s workflows to track metrics like cycle time, straight-through-processing rates, and re-open percentages.
Governance
Moxo ensures compliance and security with SSO/SAML, role-based access, HIPAA/PHI handling, and full audit exports. This means insurers can scale automation without sacrificing regulatory alignment.
Why Moxo
A well-run FNOL workflow demands more than intake forms. It requires workflow automation, branded client-facing portals, and ironclad security. With Moxo, insurers can:
- Automate approvals, reminders, and escalations through workflow automation to speed claims.
- Provide clients with a mobile-first, branded portal via Moxo’s client portal for documents, communication, and updates.
- Maintain SOC 2 and GDPR compliance with enterprise-grade security, including encryption, role-based access, and audit trails.
- Achieve measurable ROI with document collection and project management: 40–60% faster approvals, 75% more client capacity, and 95% less email.
Moxo case studies highlight real-world results. For example, a leading consulting firm reduced process length by 54% using Moxo’s workflow automation and portals. G2 reviewers consistently praise Moxo for “eliminating endless email threads” and “delivering one secure place for client interactions.”
Explore more about Moxo’s integrations with policy systems, CRMs, and payments to see how these capabilities extend beyond FNOL.
Get it right, every time
The FNOL stage defines the success of the entire claims journey. By aligning intake, verification, evidence, policy checks, severity scoring, and communication under one structured workflow, insurers can create both efficiency and trust. With platforms like Moxo, these steps become easier, faster, and more compliant—ensuring claims get the right start every time.
If you want to explore how Moxo can support your FNOL workflows, visit the get started page to book a demo.
FAQs
What is a claims processing workflow?
It’s the step-by-step process insurers use to handle claims — from intake to adjudication, payment, and closeout.
How do SLAs improve claims processing?
SLAs set time-bound expectations. With Moxo, SLAs can trigger automated escalations, ensuring no claim falls through.
Can clients track their claims online?
Yes. With a client portal, customers can submit documents, track status, and receive updates in real time.
What compliance requirements apply to claims workflows?
Insurers must comply with regulations like SOC 2, GDPR, HIPAA. Moxo’s audit trails and encryption make compliance easier.
Does Moxo replace my claims system?
No. Moxo complements policy admin and claims systems, serving as the orchestration layer for external participants and workflow automation.