Hospitals are not overwhelmed by patient volume alone.
They are overwhelmed by coordination.
Patient intake and referral workflows sit at the centre of hospital operations. They involve patients, administrative teams, clinicians, specialists, payers, and compliance functions. Every handoff introduces delay, risk, and rework.
AI automation has entered healthcare to relieve this pressure. But speed alone does not solve the problem. When automation is layered on top of fragmented execution, errors scale faster than efficiency gains.
This article examines how AI-driven hospital workflow automation changes intake and referral operations only when execution is structured, human oversight is explicit, and governance is embedded into how work actually runs.
Key takeaways
- AI-driven workflow automation can reduce patient intake processing time by up to 70% while improving data accuracy
- Automated referral validation eliminates manual errors and ensures patients reach the right specialists faster
- HIPAA-compliant AI routing protects sensitive patient data while streamlining hospital operations
- Secure collaboration platforms enable doctors, patients, and AI agents to work together seamlessly
- Modern workflow automation solutions integrate with existing hospital systems without disrupting current processes
The patient intake bottleneck
Walk into any hospital emergency department or outpatient clinic, and you'll see the same scene playing out. Patients clutching clipboards, filling out forms by hand. Registration staff manually enter information into computer systems. Phone calls back and forth to verify insurance coverage. It's a process that hasn't changed much in decades, even as technology has revolutionized almost every other aspect of our lives.
The traditional patient intake process creates several problems:
- Manual data entry errors that can lead to billing issues or even clinical mistakes
- Long wait times that frustrate patients before they even see a doctor
- Duplicate or incomplete records that complicate care coordination
- Administrative staff spend hours on repetitive tasks instead of patient interaction
- Inconsistent data collection across different departments or facilities
These inefficiencies don't just inconvenience patients. They cost the healthcare system billions of dollars annually and contribute to clinician burnout.
How AI transforms patient intake
Artificial intelligence is changing the game by automating the heavy lifting of patient intake while maintaining the accuracy and security that healthcare demands.
Intelligent data capture and Validation
Modern AI systems can automatically extract information from various sources. When a patient submits intake forms digitally, AI can read and validate the information in real time. It checks for completeness, flags inconsistencies, and even verifies that insurance information matches current coverage databases.
But it goes further than that. AI can:
- Scan uploaded insurance cards and extract policy details automatically
- Cross-reference patient information with existing medical records to prevent duplicates
- Validate addresses, phone numbers, and emergency contacts for accuracy
- Identify missing required fields and prompt patients to complete them before submission
- Translate and standardize information from different formats into a unified system
This level of automation means fewer errors make it into the system, and staff can focus on addressing genuine issues rather than data entry.
Predictive scheduling and resource allocation
AI doesn't just handle the paperwork. It can analyze intake information to predict patient needs and optimize scheduling. If a patient's symptoms suggest they'll need imaging or lab work, the system can automatically flag it and coordinate with the relevant departments. This kind of intelligent routing reduces wait times and improves the overall patient experience.
Digitizing forms is not automation.
True execution improvement requires:
- Clear ownership of each intake step
- Validation before data enters clinical systems
- Visibility into what is missing and who owns it
- Defined escalation when intake stalls
AI assists by validating information, flagging inconsistencies, and preparing data for review. Humans remain responsible for decisions and exceptions.
When intake is orchestrated, delays surface early instead of becoming clinical disruptions.
Streamlining referral management
Referrals represent another major administrative challenge in healthcare. When a primary care physician refers a patient to a specialist, multiple steps must occur correctly. The referral needs to be documented, sent to the right specialist, verified by insurance, and tracked to ensure the patient actually receives the care they need.
Too often, referrals fall through the cracks. Patients don't follow up, paperwork gets lost, or insurance denials happen weeks after the initial referral. AI-driven referral management solves these problems systematically.
Automated referral data validation
When a doctor initiates a referral, AI systems can immediately validate several critical elements:
- Whether the patient's insurance covers the specialist visit
- If prior authorization is required, automatically initiate that process
- Which specialists in the network have availability and expertise for the specific condition
- Whether all required clinical documentation is attached to support the referral
- If the patient has any existing appointments that might conflict
This validation happens in seconds rather than days, and it catches issues before they become problems for patients.
Intelligent routing and follow-up
Once validated, AI can route referrals to the most appropriate specialist based on factors like expertise, availability, location, and patient preferences. The system can also monitor whether patients actually schedule and attend their specialist appointments, sending automated reminders or alerts if follow-up is needed.
Some advanced systems even use natural language processing to analyze referral notes and match patients with specialists who have specific experience with their conditions. This kind of intelligent matching improves outcomes and reduces unnecessary consultations.
The critical importance of HIPAA compliance
Here's where things get serious. Healthcare data is among the most sensitive information that exists. Patient privacy isn't just important for ethical reasons; it's legally required under HIPAA (Health Insurance Portability and Accountability Act) and other regulations.
Any AI system handling patient intake or referrals must be built with HIPAA compliance at its core, not as an afterthought.
What HIPAA-compliant AI routing looks like
HIPAA-compliant AI systems incorporate several critical security measures:
- End-to-end encryption for all patient data in transit and at rest
- Role-based access controls that ensure only authorized personnel can view specific information
- Comprehensive audit trails that log every access and modification to patient records
- Automatic de-identification of data when used for analytics or AI training
- Business associate agreements (BAAs) that clearly define responsibilities for data protection
- Regular security assessments and penetration testing to identify vulnerabilities
The AI itself must be designed to minimize data exposure. Rather than transmitting entire medical records, properly designed systems only share the specific data elements needed for each task. When routing referrals, for example, the AI might access diagnostic codes and insurance information without needing to read detailed clinical notes.
Why security can't be compromised
Healthcare organizations face severe penalties for HIPAA violations, ranging from thousands to millions of dollars per incident. But the real cost goes beyond fines. A data breach can destroy patient trust, damage a hospital's reputation, and even put patients at risk if their medical information is compromised.
That's why healthcare leaders must be extremely careful when selecting AI workflow automation tools. The vendor needs to demonstrate not only technical capabilities but also a genuine commitment to healthcare security standards.
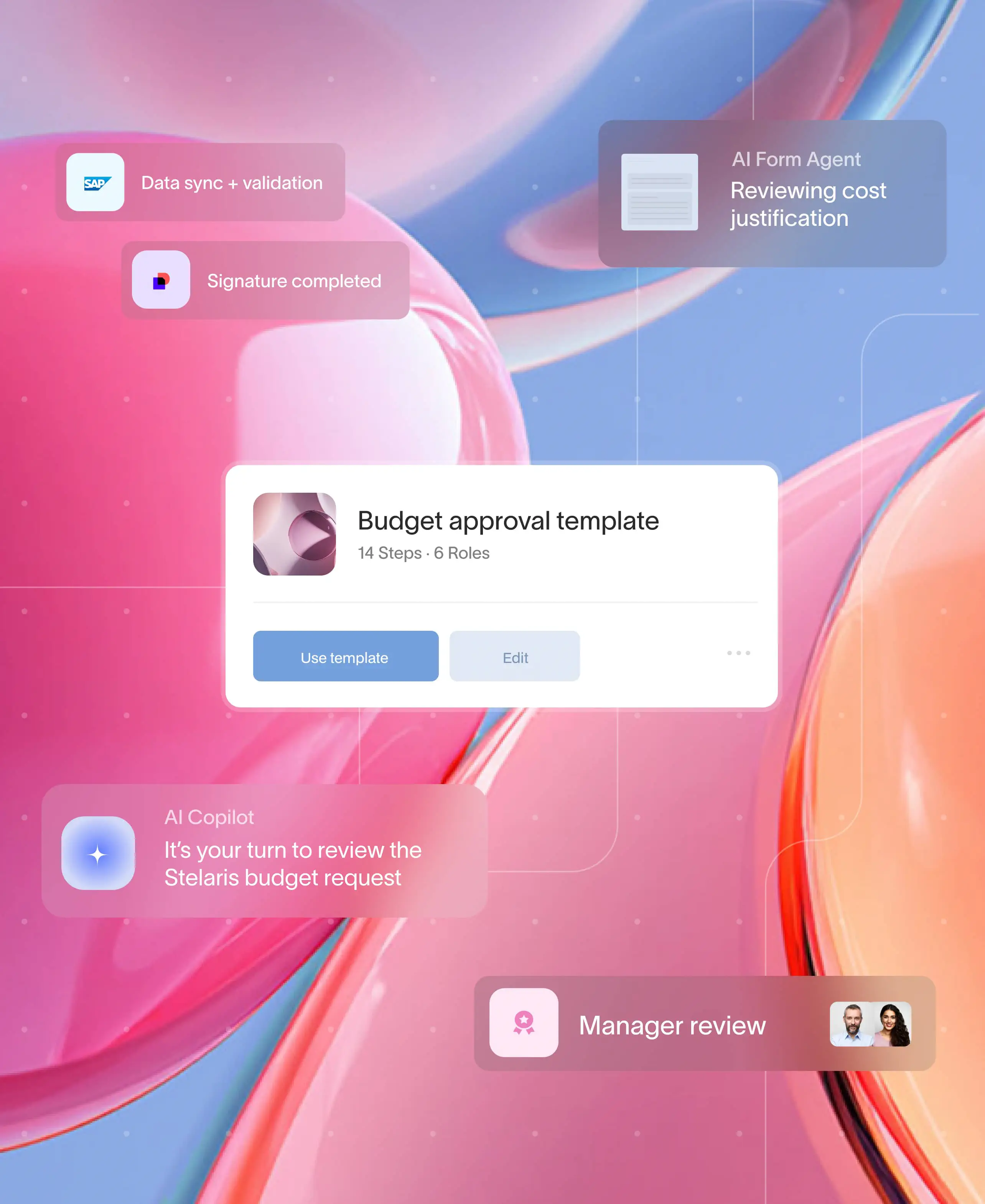
The Moxo approach: Secure collaboration at scale
While many workflow automation tools exist, few are purpose-built for the unique demands of healthcare collaboration. This is where platforms like Moxo stand out.
Moxo is a platform for orchestrating business processes. In hospital workflows, it acts as the execution layer where intake, referrals, document exchange, approvals, and AI assistance operate inside structured workflows.
AI supports preparation and validation. Humans retain decision authority.
Execution holds up because:
- Work stays inside governed flows
- Ownership is explicit at every step
- External participants are managed intentionally
- Audit trails are generated automatically
- Exceptions follow defined paths
Moxo does not replace clinical systems. It connects people, systems, and decisions into execution that survives real hospital conditions. Think of it as a HIPAA-compliant collaboration hub that brings together all the elements of patient care in one place.
How Moxo enables seamless healthcare workflows
The platform creates dedicated, encrypted workspaces for each patient case or referral. Within these workspaces:
- Patients can securely submit intake information and upload required documents
- AI agents automatically validate and process information, flagging issues for human review
- Doctors and specialists can access everything they need without switching between multiple systems
- Insurance verification and prior authorization requests happen automatically in the background
- All communication and document sharing occurs within a HIPAA-compliant environment
What makes this particularly powerful is how it reduces friction in the healthcare process. Instead of patients calling to check on referral status, or staff emailing back and forth about missing information, everything happens in a centralized, trackable workspace.
Real-world impact
Healthcare organizations using Moxo have reported significant improvements in their workflows. The platform's ability to orchestrate workflows that involve multiple stakeholders (patients, referring physicians, specialists, insurance companies, and administrative staff) while maintaining strict security standards sets it apart from generic collaboration tools.
Implementation considerations
Rolling out AI-driven workflow automation in a hospital setting requires careful planning. Here are key factors to consider:
Integration with existing systems
Most hospitals already use electronic health record (EHR) systems, practice management software, and various departmental applications. Your workflow automation solution needs to integrate with these existing tools rather than requiring a complete replacement.
Look for platforms that offer:
- APIs and pre-built connectors for common healthcare systems
- HL7 and FHIR compatibility for health data exchange
- Flexible configuration that adapts to your specific workflows
Staff training and change management
The best technology in the world won't help if your staff doesn't use it. Successful implementation requires:
- Clear communication about why changes are happening and how they'll benefit everyone
- Hands-on training that addresses real-world scenarios
- Ongoing support as staff adapt to new processes
- Feedback mechanisms to identify and address pain points quickly
Measuring success
How do you know if your workflow automation is actually working? Track metrics like:
- Time from patient arrival to completion of the intake process
- Error rates in patient data entry
- Percentage of referrals that result in completed specialist visits
- Staff hours spent on administrative tasks versus patient care
- Patient satisfaction scores related to the intake and referral experience
The future of healthcare workflow automation
We're still in the early stages of AI for healthcare workflows. As these systems become more sophisticated, we'll likely see:
- Predictive analytics that identify potential issues before they occur
- More sophisticated natural language processing that can understand complex medical terminology and context
- AI assistants that can handle patient questions and triage concerns in real time
- Seamless integration across entire healthcare networks, not just individual facilities
The key is to adopt these technologies thoughtfully, always keeping patient safety and data security at the forefront.
Transform your healthcare workflows with Moxo
The combination of AI-driven automation and secure collaboration platforms represents a genuine opportunity to improve healthcare delivery. As hospitals face increasing pressure to do more with less, these tools aren't just nice-to-haves. They're becoming essential to providing high-quality, patient-centred care in a sustainable way.
Moxo's HIPAA-compliant collaboration platform brings together patients, providers, and AI-powered automation in one secure workspace.
Get started with Moxo today and see the difference secure, intelligent workflow automation can make.
FAQs
Is AI-driven workflow automation secure enough for healthcare?
When properly implemented, AI workflow automation can actually be more secure than manual processes. HIPAA-compliant platforms use encryption, access controls, and audit trails that exceed what's possible with paper-based or simple digital systems. The key is choosing vendors who prioritize healthcare security standards and have proper certifications.
How long does it take to implement workflow automation in a hospital?
Implementation timelines vary based on the size of your organization and complexity of existing systems. Smaller clinics might deploy automation in weeks, while large hospital systems could take several months for full rollout. Phased approaches, starting with one department or workflow, often work best.
Will automation reduce the need for administrative staff?
Rather than eliminating jobs, automation typically shifts roles. Staff spend less time on repetitive data entry and more time on complex problem-solving, patient interaction, and handling exceptions that require human judgment. Many hospitals report redeploying staff to higher-value activities rather than reducing headcount.
What happens if the AI makes a mistake?
Well-designed systems include human oversight at critical points. AI can flag unusual situations for review rather than making final decisions autonomously. Additionally, audit trails allow organizations to track and correct errors quickly. The goal is to reduce errors overall, not eliminate human judgment.
Can patients still interact with real people if they need help?
Absolutely. Automation handles routine tasks, but human support remains available for questions, special circumstances, or when patients simply prefer personal interaction. The best implementations make it easy to escalate to a staff member whenever needed.