Most EHR implementations don't fail because of bad technology. They fail because of bad transitions.
Healthcare IT directors know this reality all too well. The months of planning, vendor negotiations, and staff training can unravel in a single week when the go-live day arrives without proper compliance safeguards in place. Budgets blow out. Timelines slip. Adoption stalls. And somewhere in the chaos, PHI becomes vulnerable in ways that keep compliance officers awake at night.
Healthcare go-live events are where patient safety, operational continuity, and regulatory compliance collide simultaneously. PHI is most vulnerable when moving between systems. Encryption gaps appear, temporary access rights expand, and migration errors create breach opportunities that didn't exist yesterday. The organizations that navigate these transitions successfully aren't lucky. They're deliberate. They embed HIPAA compliance into every phase as a foundational design principle, not an afterthought bolted on during the final week.
This guide breaks down exactly how to do that.
Key takeaways
PHI risk peaks during transitions: Healthcare go-live planning is uniquely high-stakes because protected health information is most exposed when data is migrating, access is temporarily expanded, and teams are working across old and new systems at once.
Compliance must be designed into the plan, not added later: HIPAA-compliant go-live execution depends on building safeguards early, including workflow mapping, encryption validation, role-based access configuration, and documented approval paths before launch.
A compliant EHR go-live checklist prevents audit gaps: The most reliable way to reduce HIPAA exposure is to use an EHR go-live checklist with explicit compliance checkpoints, required evidence, and named owners for every sign-off and control.
Multi-stakeholder coordination creates hidden exposure: Vendors, consultants, IT teams, and clinical staff can unintentionally increase PHI risk when communication and file sharing happen across email and unsecured tools, making centralized, auditable collaboration essential.
Stabilization is where compliance drift shows up: The 2–6 week post-go-live period is when workarounds, permission creep, and inconsistent PHI handling appear, so continuous monitoring and re-training are critical to sustaining compliance and adoption.
Why HIPAA compliance matters during system transitions
Healthcare system transitions create the perfect storm for compliance failures. Think about what actually happens during a go-live event. Data that lived securely in one system for years suddenly needs to move. Encryption protocols that protect PHI at rest must now protect it in transit. Access controls configured for your old system don't automatically translate to your new one.
When PHI moves between systems, your attack surface expands dramatically. Temporary access rights get granted to implementation teams, consultants, and vendor support staff. Legacy system permissions persist alongside new configurations, creating duplicate pathways to sensitive data. And in the rush to meet go-live deadlines, these gaps often go unnoticed until an auditor finds them months later.
The three HIPAA pillars all come under pressure simultaneously. The Privacy Rule governs who can access PHI during the transition. The Security Rule requires technical safeguards for ePHI in transit and at rest. The Breach Notification Rule demands incident response readiness if something goes wrong on go-live day.
With Moxo, healthcare organizations centralize all PHI-related workflows in a single HIPAA-compliant environment. Every document request, approval, and handoff is encrypted, logged, and linked to the appropriate workflow.
Moxo's security infrastructure includes SOC 2, SOC 3, and HIPAA compliance with AES-256 encryption, ensuring compliance checkpoints are embedded rather than bolted on.
Pre-go-live readiness: Building a compliant foundation
Most implementation failures share a common root cause. Organizations treat go-live as an event rather than a process. The work that determines success happens before anyone flips the switch.
Workflow mapping failures create costly rework. HealthIT.gov research confirms that organizations skipping workflow mapping must go back after go-live to fix processes, struggling to recover from productivity drops. Map clinical and operational workflows before EHR selection. Every practice setup is different, and vendor templates are starting points, not solutions.
Conduct Day-in-the-Life exercises to simulate real clinical scenarios with actual staff. For a deeper dive into optimizing clinical processes, explore workflow analysis in healthcare.
Data migration isn't just IT work. Incomplete or inaccurate data doesn't get fixed during migration. It gets migrated. Every duplicate record, missing field, and formatting inconsistency travels from your legacy system into your new environment. Implement encrypted channels for all PHI transfers and create comprehensive audit trails documenting every data movement.
Access control configuration protects against long-term exposure. HIPAA's "minimum necessary" standard doesn't pause during implementations. Configure role-based access before go-live. Establish temporary access protocols for support teams with explicit expiration dates. Document every permission change with automatic audit logging.
The EHR go-live checklist: Critical compliance checkpoints
Compliance officers need actionable frameworks, not theory. The following checkpoints should guide your transition.
Pre-go-live preparation (T-minus 2 weeks) requires verifying all interfaces for lab, imaging, and pharmacy systems are built, tested, and secure. Confirm encryption protocols are active for data in transit and at rest. Complete user acceptance testing with compliance validation. Train super-users on PHI handling during the transition period. Establish downtime procedures with paper-based backup protocols.
Go-live day execution demands heightened monitoring for PHI access patterns. Deploy at-the-elbow support with clear escalation pathways. Maintain real-time audit logging across all system interactions. Keep legacy system access available with controlled read-only permissions.
Post-go-live stabilization requires monitoring for workflow adoption gaps and PHI handling errors. Conduct daily compliance checkpoints during the stabilization period, typically 2-6 weeks. Begin training 2-3 weeks before implementation, with re-training continuing for 6-10 weeks post-go-live.
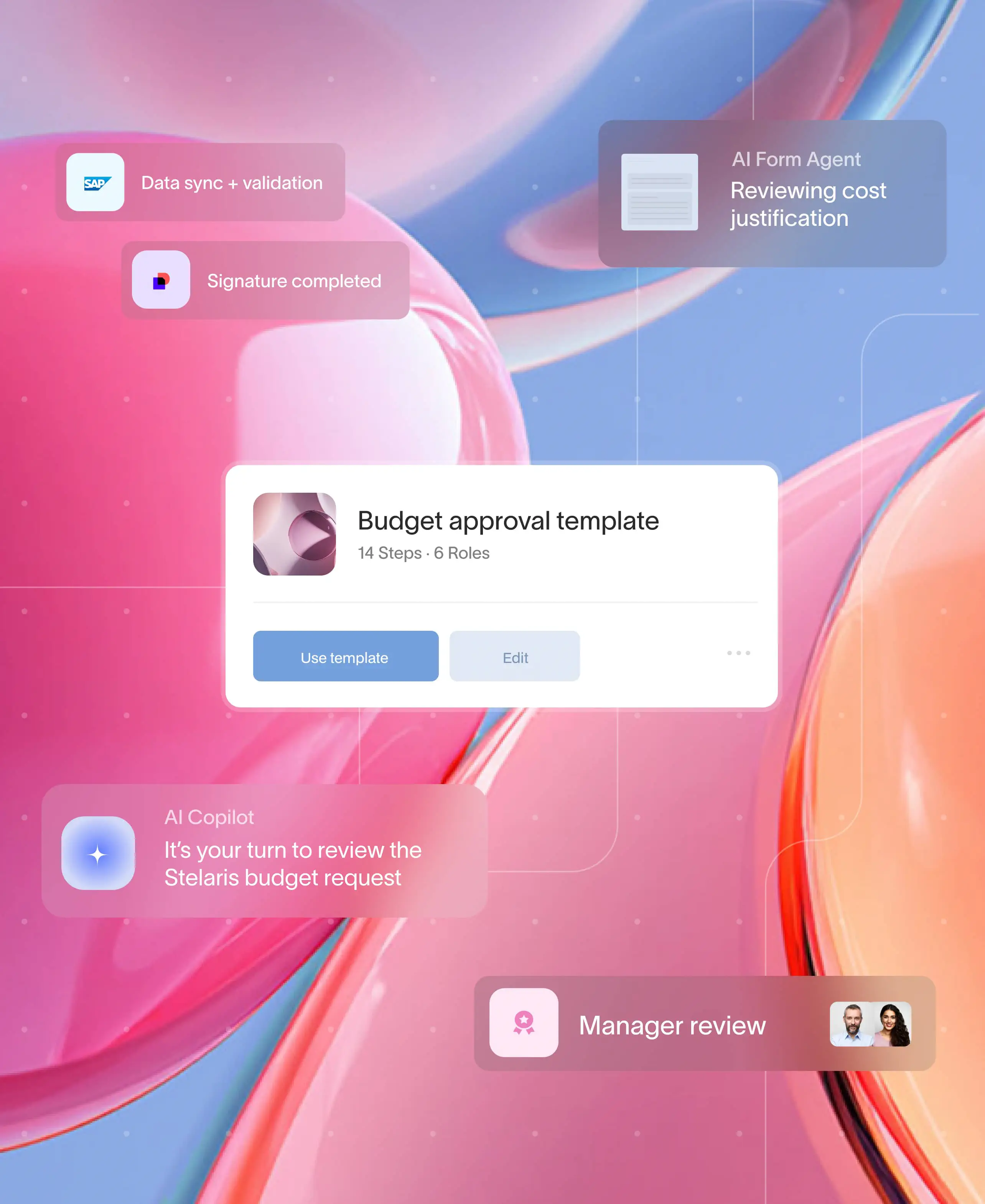
Moxo's healthcare workflow automation capabilities help organizations automate these checkpoints. Automated reminders ensure nothing falls through the cracks, while real-time notifications keep every stakeholder informed of their responsibilities.
Coordinating stakeholders without compromising compliance
Healthcare go-lives involve a sprawling cast of stakeholders. IT teams, clinical staff, compliance officers, EHR vendors, integration consultants, and external partners each create potential PHI exposure if not managed through secure channels.
The common failure mode is scattered communication via email, unsecured file sharing, and undocumented approvals. A mid-sized outpatient clinic relied on email chains for PHI access requests. When auditors demanded proof of authorization, the compliance team spent weeks reconstructing approvals from inboxes and spreadsheets.
Centralize all implementation communication in a single, auditable workspace. Require digital signatures and timestamped approvals for critical milestones. Enforce role-based visibility so consultants see only what's necessary for their scope.
Learn more about structuring these processes in our guide to client management processes.
With Moxo, healthcare organizations manage multi-stakeholder coordination through the healthcare solutions platform with built-in role-based access controls.
A healthcare billing firm implementing Moxo's digital intake forms and automated document checks reduced missing-data rejections by 42% within the first quarter.
How Moxo streamlines healthcare go-live coordination
Healthcare system transitions fail when coordination breaks down. Teams juggle email threads, chase approvals manually, and lose track of critical tasks across disconnected tools. Moxo brings every stakeholder, document, and workflow into a single HIPAA-compliant platform purpose-built for complex, multi-party processes.
Magic links eliminate access friction during critical moments. When clinical staff, vendor consultants, or compliance reviewers need to complete urgent tasks, they shouldn't be hunting for login credentials.
Moxo automatically sends secure magic links that allow stakeholders to view and complete tasks directly in the browser without logging in. During go-live week, when every hour matters, this removes the friction that causes delays and missed deadlines.
Automated reminders keep implementation timelines on track. Manual follow-ups consume hours that implementation teams don't have. Moxo sends automated reminders for pending approvals, incomplete forms, and upcoming deadlines. No one needs to chase emails or wonder who dropped the ball. The system nudges the right people at the right time, ensuring compliance checkpoints don't slip through the cracks.
Mobile access enables real-time response from anywhere. Go-live events don't pause when stakeholders leave their desks. Moxo's mobile app gives clinical leaders, IT directors, and compliance officers real-time access to approve documents, review status updates, and respond to escalations from anywhere. When an issue surfaces at 2 AM on go-live weekend, decision-makers can act immediately.
Timelines and to-dos create visibility across every workstream. Healthcare implementations involve dozens of parallel tasks across multiple teams. Moxo's timeline view shows exactly where each workstream stands, who owns what, and which tasks are blocking progress. Compliance officers see the full picture without scheduling status meetings or compiling spreadsheet updates.
AI agents handle repetitive coordination tasks. Moxo AI embeds intelligent agents directly within workflows to review form submissions, validate document completeness, and flag exceptions before they become problems.
During high-volume go-live periods, AI agents handle the manual verification work that would otherwise overwhelm your team, freeing staff to focus on issues that require human judgment.
Digital forms standardize data collection across stakeholders. Vendor attestations, access requests, training acknowledgments, and compliance sign-offs all require structured data.
Moxo's forms capture this information consistently, route it to the right approvers automatically, and log every submission for audit purposes. No more chasing PDF attachments or deciphering handwritten responses.
Integrated messaging keeps conversations in context. When questions arise about a specific document or approval, the discussion shouldn't scatter across email, Slack, and text messages.
Moxo's built-in messaging ties every conversation to the relevant workflow, creating a complete record of who said what and when. Auditors see the full context, not fragments.
Meeting scheduling and call recordings capture critical decisions. Implementation decisions made in meetings often get lost or disputed later. Moxo enables meeting scheduling directly within workflows, with call recordings and transcripts automatically linked to the relevant project.
When questions arise during stabilization about what was agreed during go-live planning, the answer is documented and searchable.
Explore how Moxo's healthcare solutions can transform your next system implementation.
Conclusion
Healthcare go-live planning isn't a one-time project. It's a compliance posture that determines whether your organization navigates transitions with audit findings, breach risks, and operational chaos, or with confidence and continuity. The organizations succeeding in 2025 embed HIPAA requirements into every phase, from workflow mapping through stabilization.
Moxo helps healthcare organizations transform fragmented implementation coordination into structured, HIPAA-compliant workflows. With secure document collection, automated approval routing, immutable audit trails, and role-based access controls, compliance becomes embedded in daily operations rather than reconstructed for auditors.
Ready to streamline your next healthcare implementation? Get started with Moxo and see how workflow orchestration keeps your go-live compliant from day one.
FAQs on healthcare go-live planning
What is a healthcare go-live event?
A healthcare go-live is when a new clinical or operational system becomes active in production. With Moxo, teams coordinate go-live through secure workflows that manage tasks, approvals, and PHI exchanges in one workspace. Learn more about Moxo healthcare solutions.
How long does stabilization last after an EHR go-live?
Most organizations plan 2–6 weeks of stabilization, with training reinforcement often extending longer. Moxo helps run hypercare through structured workflows, daily checkpoints, and real-time visibility.
What are the biggest HIPAA risks during healthcare system transitions?
Key risks include PHI exposure during migration, temporary permissions not being revoked, and missing audit trails. Moxo reduces risk with role-based access, secure file exchange, and audit logging in a HIPAA-aligned environment.
What causes most healthcare implementation failures?
Common causes include skipped workflow mapping, siloed communication, rushed change management, and unclear ownership. Moxo helps by centralizing coordination, enforcing accountability, and keeping approvals and handoffs traceable inside one workflow.
Can Moxo integrate with existing EHR and healthcare systems?
Yes. Moxo connects via APIs, webhooks, and integrations so teams can route data, trigger workflow steps, and keep documents in sync without manual follow-ups. This helps reduce tool sprawl during go-live.